Pancreatitis is inflammation of the pancreas. The pancreas plays an important role in the regulation of blood glucose levels through the production of hormones, as well as in digestion, through the production of enzymes that break down food in the small intestine. Pancreatitis occurs when the pancreatic enzymes that digest food are activated in the pancreas instead of the small intestine, causing the pancreas to digest, or break down, its own tissue . Pancreatitis can be acute, beginning suddenly and lasting a few days, or chronic, occurring over many years.
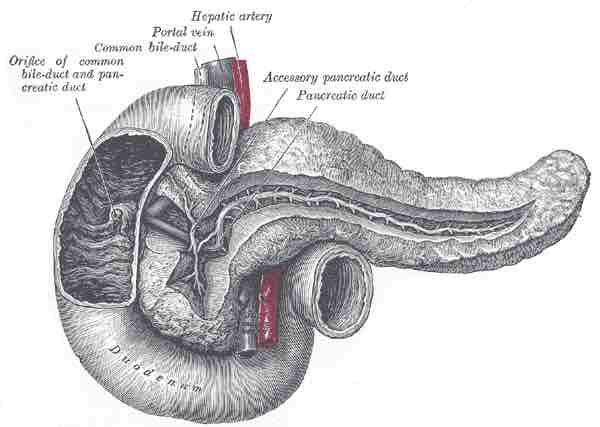
The Pancreatic Duct
The pancreas connects to the small intestine via the pancreatic duct. A blockage in this duct can cause pancreatitis.
Symptoms and Causes
The most common symptoms of pancreatitis are severe upper-abdominal burning pain radiating to the back, nausea, and vomiting that worsens with eating. Unexplained weight loss may occur from decreased amounts of pancreatic enzymes hindering digestion.
Eighty percent of pancreatitis cases are caused by alcohol and gallstones. Gallstones are the single most common cause of acute pancreatitis, while alcohol is the single most common cause of chronic pancreatitis. Pancreatitis can be caused by certain medications, as well as trauma, mumps, autoimmune disease, genetic predisposition, scorpion stings, high blood calcium, high blood triglycerides, hypothermia, certain viruses, bacteria and fungi, and less commonly, pancreatic cancer.
Treatment
The treatment of pancreatitis is supportive and depends on the severity of the illness. Mild pancreatitis treatment typically involves restriction of foods to avoid production of digestive enzymes, and administration of opiate-based painkillers. Severe pancreatitis is a serious medical emergency, and patients are typically admitted to an intensive care unit with some level of hypovolemic shock. Treatment is still supportive, with the aim of eliminating the underlying cause of the pancreatitis.
Complications and Prognosis
Early complications of pancreatitis include shock, infection, systemic inflammatory response syndrome, low blood calcium, high blood glucose, and dehydration. Blood loss, dehydration, and fluid leaking into the abdominal cavity can lead to kidney failure. Respiratory complications are often severe. Fluid in the lungs is usually present, and shallow breathing from pain can lead to lung collapse. Pancreatic enzymes may enter the blood stream and attack the lungs, causing inflammation.
Late complications include recurrent pancreatitis and the development of pancreatic pseudocyst, which are collections of pancreatic secretions that have been walled off by scar tissue. These may cause pain, become infected, rupture and bleed, block the bile duct and cause jaundice, or migrate around the abdomen.
Prognosis is generally good for mild pancreatitis. Severe pancreatitis has high mortality rates, especially where the pancreatic enzymes have begun to kill off parts of the pancreas, causing tissue necrosis.