Escherichia coli (E. coli) is a Gram-negative, rod-shaped bacterium that is commonly found in the lower intestine of warm-blooded organisms (endotherms). Most E. coli strains are harmless, but some serotypes are pathogenic and can cause serious food poisoning in humans and other species. The harmless strains are part of the normal flora of the gut, and can benefit their hosts by producing vitamin K2, and by preventing the establishment of pathogenic bacteria within the intestine.
Pathogenic E. coli
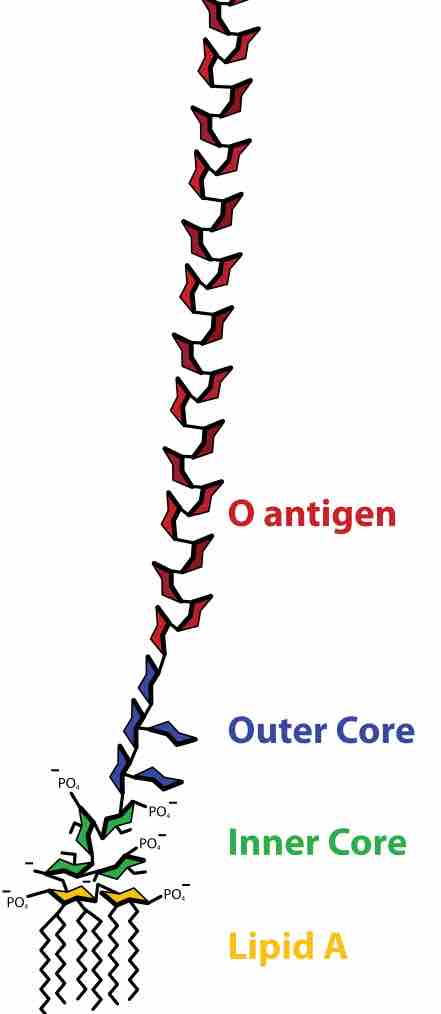
Pathogenic E. coli strains can be categorized based on elements that can elicit an immune response in animals, namely: O antigen, K antigen, H antigen, and F antigen in the lipopolysaccharide (LPS) molecules found in the outer membrane of the E. coli cell. The O antigen is a polymer of immunogenic repeating oligosaccharides which is used for serotyping E.coli. It should be noted though that antibodies towards several O antigens cross-react with other O antigens and partially to K antigens not only from E. coli, but also from other Escherichia species and Enterobacteriaceae species. There are two separate groups of K-antigen groups, named group I and group II (while a small in-between subset (K3, K10, and K54/K96) has been classified as group III). Group I consists of 100 kDa (large) capsular polysaccharides, while those in Group II, associated with extraintestinal diseases, are under 50 kDa in size.
Lipopolysaccharide
Structure of a lipopolysaccharide showing the O antigen, core region and lipid A.
In humans and in domestic animals, virulent strains of E. coli can cause various diseases. In humans, gastroenteritis, urinary tract infections, and neonatal meningitis can occur. In rarer cases, virulent strains are also responsible for haemolytic-uremic syndrome, peritonitis, mastitis, septicemia, and Gram-negative pneumonia. Certain strains of E. coli produce potentially lethal toxins. Food poisoning caused by E. coli can result from eating unwashed vegetables or undercooked meat. If E. coli bacteria escape the intestinal tract through a perforation (for example from an ulcer, a ruptured appendix, or due to a surgical error) and enter the abdomen, they usually cause peritonitis that can be fatal without prompt treatment.
Transmission of pathogenic E. coli often occurs via fecal–oral transmission. Common routes of transmission include unhygienic food preparation, farm contamination due to manure fertilization, irrigation of crops with contaminated greywater or raw sewage, feral pigs on cropland, or direct consumption of sewage-contaminated water. According to the U.S. Food and Drug Administration, the fecal-oral cycle of transmission can be disrupted by cooking food properly, preventing cross-contamination, instituting barriers such as gloves for food workers, instituting health care policies so food industry employees seek treatment when they are ill, pasteurization of juice or dairy products and proper hand washing requirements.
Uropathogenic E. coli
Uropathogenic E. coli (UPEC) is responsible for approximately 90% of urinary tract infections (UTI) seen in individuals with ordinary anatomy. In ascending infections, fecal bacteria colonize the urethra and spread up the urinary tract to the bladder, as well as to the kidneys (causing pyelonephritis), or the prostate in males. Because women have a shorter urethra than men, they are 14 times more likely to suffer from an ascending UTI. Uropathogenic E. coli use P fimbriae (pyelonephritis-associated pili) to bind urinary tract endothelial cells and colonize the bladder. UPEC can evade the body's innate immune defences (e.g. the complement system) by invading superficial umbrella cells to form intracellular bacterial communities (IBCs). They also have the ability to form K antigen, capsular polysaccharides that contribute to biofilm formation. Descending infections in turn, though relatively rare, occur when E. coli cells enter the upper urinary tract organs (kidneys, bladder or ureters) from the blood stream.
E. coli and Meningitis
Neonatal meningitis is produced by a serotype of E. coli that contains a capsular antigen called K1. The colonization of the newborn's intestines with these stems, that are present in the mother's vagina, lead to bacteraemia, which leads to meningitis. Severe meningitis in the neonates are caused because of the absence of the IgM antibodies from the mother (these do not cross the placenta because FcRn only mediates the transfer of IgG), plus the fact that the body recognizes as self the K1 antigen, as it resembles the cerebral glicopeptides. In stool samples, microscopy will show Gram-negative rods, with no particular cell arrangement.
Treating E. coli
Bacterial infections are usually treated with antibiotics. However, the antibiotic sensitivities of different strains of E. coli vary widely. As Gram-negative organisms, E. coli are resistant to many antibiotics that are effective against Gram-positive organisms. Antibiotics which may be used to treat E. coli infection include amoxicillin, as well as other semisynthetic penicillins, many cephalosporins, carbapenems, aztreonam, trimethoprim-sulfamethoxazole, ciprofloxacin, nitrofurantoin, and the aminoglycosides. Researchers have actively been working to develop safe, effective vaccines to lower the worldwide incidence of E. coli infection.