The Human Microbiome Project
The Human Microbiome Project (HMP) is a United States National Institutes of Health initiative aimed at identifying and characterizing the microorganisms which are found in association with both healthy and diseased humans .
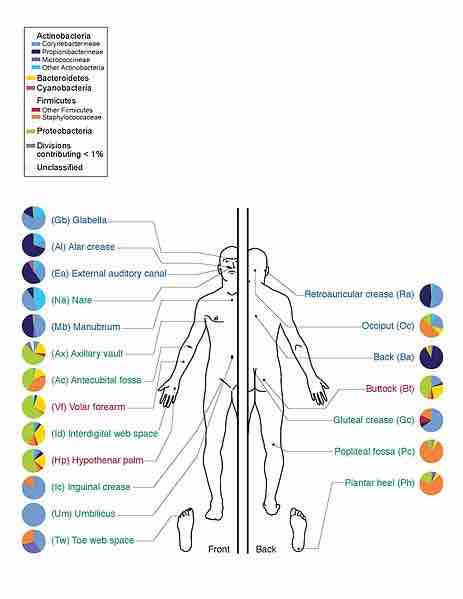
Bacteria commonly found in and on humans
This is a depiction of the human body and bacteria that predominates throughout it.
Total microbial cells found in association with humans may exceed the total number of cells making up the human body by a factor of ten-to-one. The total number of genes associated with the human microbiome could exceed the total number of human genes by a factor of 100-to-one.
Organisms expected to be found in the human microbiome may generally be categorized as bacteria (the majority), archaea, yeasts, and single-celled eukaryotes as well as various helminth parasites and viruses, such as those that infect cellular microbiome organisms.
The HMP project discovered several "surprises", including:
- Bacterial protein-coding genes are estimated as 360 times more abundant than human genes.
- Microbial metabolic activities, for example, digestion of fats, are not always provided by the same bacterial species.
- Components of the human microbiome change over time, affected by a patient disease state and medication.
Examples of Non-pathogenic Interactions
Gut flora consists of microorganisms that live in the digestive tracts of animals and is the largest reservoir of human flora. The human body, consisting of about 10 trillion cells, carries about ten times as many microorganisms in the intestines. The metabolic activities performed by these bacteria resemble those of an organ, leading some to liken gut bacteria to a "forgotten" organ.
Bacteria make up most of the flora in the colon and up to 60% of the dry mass of feces. Between 300 and 1000 different species live in the gut. It is probable that 99% of the bacteria come from about 30 or 40 species. Fungi and protozoa also make up a part of the gut flora, but little is known about their activities.
The relationship between gut flora and humans is thought to be not merely commensal, but rather a mutualistic relationship. Though people can survive without gut flora, the microorganisms perform a host of useful functions, such as fermenting unused energy substrates, training the immune system, preventing growth of harmful, pathogenic bacteria, regulating the development of the gut, producing vitamins for the host, and producing hormones to direct the host to store fats. In certain conditions, some species can cause disease by producing infection or increasing the host's cancer risk.
The skin microbiota are composed mostly of bacteria of which there are around 1000 species upon human skin from 19 phyla. The total number of bacteria on an average human has been estimated at 1012.
Skin flora are usually non-pathogenic and either commensal or mutualistic. The benefits of bacteria include preventing transient pathogenic organisms from colonizing the skin surface, either by competing for nutrients, secreting chemicals against them, or stimulating the skin's immune system. Resident microbes can cause skin diseases and enter the blood system creating life-threatening diseases particularly in immunosuppressed people .
Pathogenic Interactions
Among the almost infinite varieties of microorganisms, relatively few cause disease in otherwise healthy individuals. Infectious disease results from the interplay between those few pathogens and the defenses of the hosts they infect. Infectious diseases comprise clinically evident illness resulting from the infection, and the presence and growth of pathogenic biological agents in an individual host organism. Infectious pathogens include some viruses, bacteria, fungi, protozoa, multicellular parasites, and aberrant proteins known as prions. Primary pathogens cause disease as a result of their presence or activity within the normal, healthy host. Their intrinsic virulence is due to their need to reproduce and spread .

The malaria plasmodium
Malaria is transmitted to people and animals by mosquitoes. Malarial sporozoites develop inside oocysts and are released in large numbers into the hemocoel of Anopheles stephensi mosquitoes. This false-colored electron micrograph shows a sporozoite migrating through the cytoplasm of midgut epithelia.
Organisms which cause an infectious disease in a host with depressed resistance are classified as opportunistic pathogens. Opportunistic disease may be caused by microbes that are ordinarily in contact with the host, such as pathogenic bacteria or fungi in the gastrointestinal tract. They may also result from (otherwise innocuous) microbes acquired from other hosts or from the environment as a result of traumatic introduction (as in surgical wound infections). An opportunistic disease requires impairment of host defenses, which may occur as a result of genetic defects, exposure to antimicrobial drugs or immunosuppressive chemicals, exposure to ionizing radiation, or as a result of an infectious disease with immunosuppressive activity.
The success of any pathogen depends on its ability to elude host immune responses. Therefore, pathogens evolved several methods that allow them to successfully infect a host, while evading the immune system. Bacteria often overcome physical barriers by secreting enzymes that digest the barrier. An evasion strategy used by several pathogens to avoid the innate immune system is to hide within the cells of their host. The mechanisms used to evade the adaptive immune system are more complicated. The simplest approach is antigenic variation: rapid changes of non-essential epitopes on the surface of the pathogen, while keeping essential epitopes concealed.