Major histocompatibility complex (MHC) is a cell-surface molecule encoded by a large gene family in all vertebrates. MHC molecules mediate interactions of leukocytes with other leukocytes or body cells. MHC determines compatibility of donors for organ transplant as well as one's susceptibility to an autoimmune disease via cross-reacting immunization. In humans, MHC is also called human leukocyte antigen (HLA), because MHC can often act as an antigen for human leukocytes.
Types of MHC
MHC is a polymorphic protein attached to the surface of cells. Three different classes of MHC differ in structure and function in the immune system, but are all encoded by the same set of gene sequences.
- MHC I is presented on all cells of the body. It contains an epitope that forms the structural binding site for an antigen. MHC I interacts with natural killer (NK) cells and cytotoxic T cells to signal whether a cell is self or non-self, and whether it contains an antigen specific to that T cell.
- MHC II is presented mainly on macrophages, dendritic cells, and helper T cells, which are all involved in antigen presentation. It has a longer helical region than MHC I, which allows it to bind to CD4 (helper T cells) during antigen presentation.
- MHC III is a secreted enzyme that is neither membrane-bound nor involved in antigen presentation like MHC I and II. It is merely included as an MHC protein because it is encoded by the same set of genes. It is involved in production of complement proteins and inflammatory cytokines.
During antigen processing prior to presentation, protein peptides from pathogens and MHC (I or II) travel through the cytoplasm and then to the cell membrane surface. A complex series of vesicles enables MHC transport from the cell, and the endoplasmic reticulum and Golgi bodies facilitate this transport during antigen processing. After processing, the MHC can present the peptide antigen bound to it to naive T cells.
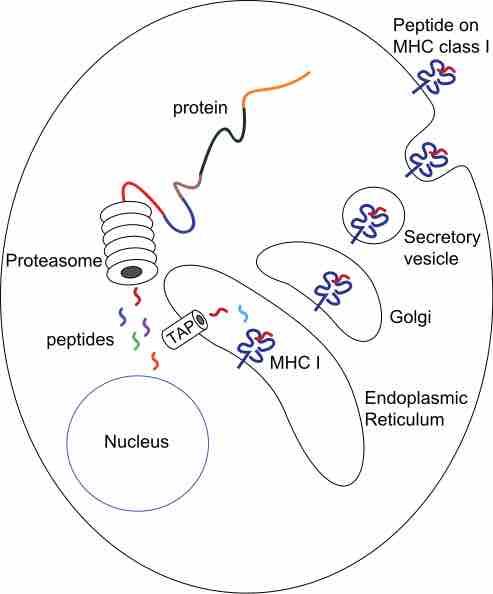
MHC Class I processing
MHC class I pathway: proteins in the cytosol are degraded by the proteasome, liberating peptides internalized by TAP channel in the endoplasmic reticulum, there associating with MHC-I molecules freshly synthesized. MHC-I/peptide complexes enter Golgi apparatus, are glycosylated, enter secratory vesicles, fuse with the cell membrane, and externalize on the cell membrane interacting with T lymphocytes.
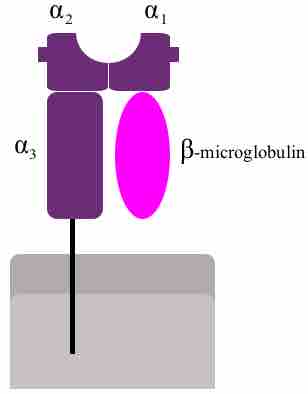
MHC Class I
MHC class I protein molecule.
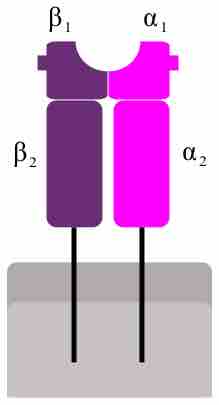
MHC Class II
MHC class II protein molecule.
HLA and Organ Rejection
Organ transplantation is a complex procedure that can potentially cure many chronic diseases and acute injuries. However, surgically-replaced organs are often rejected by the body's immune system. MHC is also called human leukocyte antigen (HLA) and varies considerably among different members of the same species. If the T and B cells of the body recognize the HLA of the graft as foreign, they will attack the organ graft. The damage in organ rejection can be acute or chronic, cell-mediated or antibody-mediated, and often involves diffuse damage of the graft that cause necrosis and infarction (tissue death from lack of oxygen) to the graft tissue by attacking its vascular components.
In nearly all cases, immunosuppressive chemotherapy is a requirement for successful organ transplantation. These drugs can stop acute organ rejection after the procedure, but will not stop chronic organ rejection, in which gradual vascular lesions and endothelial thickening slowly kill the graft. If an organ donor has HLA similar to that of the recipient, the risk of organ rejection is reduced. However this isn't feasible for heart, liver, or lung transplants because there generally isn't enough time in these cases to find a matching organ donor.