Extracellular fluid is separated among the various compartments of the body by membranes. These membranes are hydrophobic and repel water, however there a few ways that fluids can move between body compartments. Small gaps in membranes, such as the tight junctions, allow fluids and some of their contents to pass through membranes by way of pressure gradients.
Formation of Interstitial Fluid
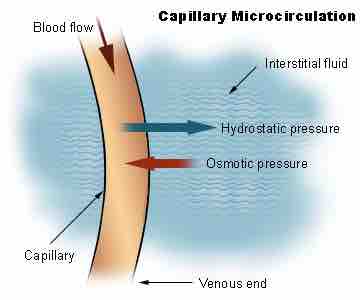
Hydrostatic pressure is generated by the contractions of the heart during systole. It pushes water out of small tight junctions in the capillaries. The water potential is created due to the ability of small solutes to pass through the walls of capillaries. This buildup of solutes induces osmosis. The water passes from a high concentration (of water) outside of the vessels to a low concentration inside of the vessels, in an attempt to reach an equilibrium. The osmotic pressure drives water back into the vessels. Because the blood in the capillaries is constantly flowing, equilibrium is never reached.
The balance between the two forces differs at different points on the capillaries. At the arterial end of a vessel, the hydrostatic pressure is greater than the osmotic pressure, so the net movement favors water and other solutes being passed into the tissue fluid. At the venous end, the osmotic pressure is greater, so the net movement favors substances being passed back into the capillary. This difference is created by the direction of the flow of blood and the imbalance in solutes created by the net movement of water favoring the tissue fluid.
Removal of Interstitial Fluid
To prevent a build up of tissue fluid surrounding the cells in the tissue, the lymphatic system plays a part in the transport of tissue fluid. Tissue fluid can pass into the surrounding lymph vessels, and eventually ends up rejoining the blood. Sometimes the removal of tissue fluid does not function correctly, and there is a build-up, which is called edema. Edema is responsible for the swelling that occurs during inflammation, and in certain diseases in which lymphatic drainage pathways are obstructed.
Starling Equation
Capillary permeability can be increased by the release of certain cytokines, anaphylatoxins, or other mediators (such as leukotrienes, prostaglandins, histamine, bradykinin, etc. ) which are released by cells during inflammation. The Starling equation defines the forces across a semipermeable membrane and allows calculation of the net flux. The solution to the equation is known as the net filtration or net fluid movement. If positive, fluid will tend to leave the capillary (filtration). If negative, fluid will tend to enter the capillary (absorption). This equation has a number of important physiologic implications, especially when disease processes grossly alter one or more of the variables.

The Starling Model
Note the concentration of interstitial solutes (orange) increases proportionally to the distance from the arteriole.
According to Starling's equation, the movement of fluid depends on six variables :
Capillary Dynamics
Oncotic pressure exerted by proteins in blood plasma tends to pull water into the circulatory system.
- Capillary hydrostatic pressure ( Pc )
- Interstitial hydrostatic pressure ( Pi )
- Capillary oncotic pressure ( πz )
- Interstitial oncotic pressure ( πi )
- Filtration coefficient ( Kf )
- Reflection coefficient ( σ )
The Starling Equation is mathematically described as Flux=Kf[(Pc-Pi)-σ (πz-πi )].