The old model: Lymphoid vs Myeloid ( and ). This model of lymphopoiesis had the virtue of relative simplicity and agreement with nomenclature and terminology; also, it is essentially valid for the favorite lab animal, the mouse. pHSC pluripotent, self-renewing, hematopoietic stem cells give rise to MPP multipotent progenitors (these give rise to ELP, or PRO, Prolymphocytes); early lymphoid progenitors; and finally to the CLP Common lymphoid progenitor, a cell type fully committed to the lymphoid lineage. pHSC, MPP and ELP cells are not fully committed to the lymphoid lineage because if one is removed to a different location, it may differentiate into non-lymphoid progeny. However, CLP are committed to the lymphoid lineage. The CLP is the transit cell responsible for these (generally parallel) stages of development, below:
NK cells Dendritic cells (lymphoid lineage; DC2) Progenitor B cells Pro-B cells => Early Pro (or pre-pre)-B cells => Late Pro (or pre-pre)-B cells Large Pre-B cells => Small Pre-B cells Immature B cells B Cells => (B1 cells; B2 cells) Plasma cells Pro-T cells T-cells.
Developmental Immunology
The body's capability to react to antigen depends on a person's age, antigen type, maternal factors and the area where the antigen is presented. Neonates are said to be in a state of physiological immunodeficiency, because both their innate and adaptive immunological responses are greatly suppressed. Once born, a child's immune system responds favorably to protein antigens while not as well to glycoproteins and polysaccharides. In fact, many of the infections acquired by neonates are caused by low virulence organisms like Staphylococcus and Pseudomonas.
In neonates, opsonic activity and the ability to activate the complement cascade is very limited. For example, the mean level of C3 in a newborn is approximately 65% of that found in the adult. Phagocytic activity is also greatly impaired in newborns. This is due to lower opsonic activity, as well as diminished up-regulation of integrin and selectin receptors, which limit the ability of neutrophils to interact with adhesion molecules in the endothelium.
Their monocytes are slow and have a reduced ATP production, which also limits the newborns phagocytic activity. Although the number of total lymphocytes is significantly higher than in adults, the cellular and humoral immunity is also impaired. Antigen presenting cells in newborns have a reduced capability to activate T cells. Also, T cells of a newborn proliferate poorly and produce very small amounts of cytokines like IL-2, IL-4, IL-5, IL-12, and IFN-g which limits their capacity to activate the humoral response as well as the phagocitic activity of macrophage. B cells develop early in gestation but are not fully active.
Maternal factors also play a role in the body's immune response. At birth most of the immunoglobulin is present is maternal IgG. Because IgM, IgD, IgE and IgA don't cross the placenta, they are almost undetectable at birth. Although some IgA is provided in breast milk. These passively acquired antibodies can protect the newborn up to 18 months, but their response is usually short-lived and of low affinity. These antibodies can also produce a negative response. If a child is exposed to the antibody for a particular antigen before being exposed to the antigen itself then the child will produce a dampened response. Passively acquired maternal antibodies can suppress the antibody response to active immunization. Similarly the response of T-cells to vaccination differs in children compared to adults, and vaccines that induce Th1 responses in adults do not readily elicit these same responses in neonates. By 6-9 months after birth, a child's immune system begins to respond more strongly to glycoproteins. Not until 12-24 months of age is there a marked improvement in the body's response to polysaccharides. This can be the reason for the specific time frames found in vaccination schedules.
During adolescence the human body undergoes several physical, physiological and immunological changes. These changes are started and mediated by different hormones. Depending on the sex either testosterone or 17-β-oestradiol, act on male and female bodies accordingly, start acting at ages of 12 and 10 years. There is evidence that these steroids act directly not only on the primary and secondary sexual characteristics, but also have an effect on the development and regulation of the immune system. There is an increased risk in developing autoimmunity for pubescent and post pubescent females and males. There is also some evidence that cell surface receptors on B cells and macrophages may detect sex hormones in the system.
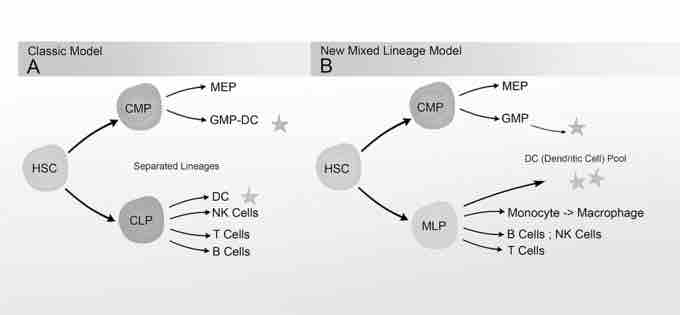
New Mixed Myeloid-Lymphoid Progenitor Tree(RCCH) Grayscale
Side by side comparison of the new and old lineage models.
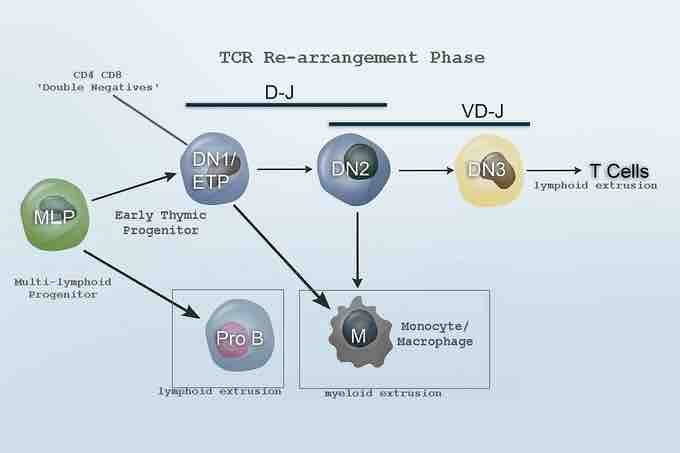
Revised Lineage Myelo-lymphoid flowchart.
Revised Lineage Myelo-lymphoid flowchart.