A peptic ulcer, also known as peptic ulcer disease, is an erosion in the wall of the stomach, duodenum, or esophagus . As many as 70–90% of such ulcers are associated with Helicobacter pylori, a spiral-shaped bacterium that lives in the acidic environment of the stomach. Ulcers can also be caused or worsened by drugs such as aspirin, ibuprofen, and other NSAIDs.
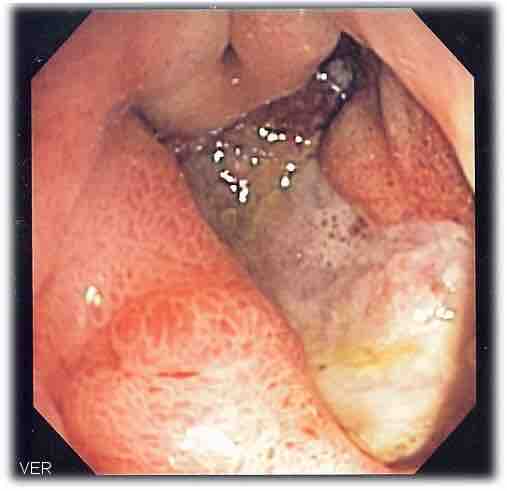
Deep gastric ulcer
This image, acquired via endoscope, shows a deep gastric ulcer.
Symptoms
Symptoms of a peptic ulcer include abdominal pain, classically near the stomach with severity relating to mealtimes, about three hours after eating a meal; bloating and abdominal fullness; nausea; copious vomiting; loss of appetite and weight loss; vomiting of blood; and melena, which are tarry, foul-smelling feces due to oxidized iron from hemoglobin. Rarely, an ulcer can lead to a gastric or duodenal perforation, which leads to acute peritonitis. This is extremely serious and requires immediate surgery.
Causes
A major causative factor of ulcers is chronic inflammation due to Helicobacter pylori that colonizes the mucosa. The immune system is unable to clear the infection, despite the appearance of antibodies. Thus, the bacterium can cause a chronic active gastritis, resulting in a defect in the regulation of gastrin production by that part of the stomach. Gastrin secretion can either be increased, or as in most cases, decreased, resulting in a too basic or too acidic stomach environment, respectively. A decrease in acid can promote H. pylori growth and an increase in acid can contribute to the erosion of the mucosa and therefore ulcer formation.
Another major cause is the use of NSAIDs. The gastric mucosa protects itself from gastric acid with a layer of mucus, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (cox-1), which is essential for the production of these prostaglandins.
Researchers also continue to look at stress as a possible cause, or at least complication, in the development of ulcers. There is debate as to whether psychological stress can influence the development of peptic ulcers. Burns and head trauma, however, can lead to physiologic stress ulcers, which are reported in many patients who are on mechanical ventilation.
Diagnosis
The diagnosis is mainly established based on the characteristic symptoms. Stomach pain is usually the first signal of a peptic ulcer. In some cases, doctors may treat ulcers without diagnosing them with specific tests and observe whether the symptoms resolve, this indicating that their primary diagnosis was accurate.
Confirmation of the diagnosis is made with the help of tests such as endoscopies or barium contrast x-rays. The tests are typically ordered if the symptoms do not resolve after a few weeks of treatment. Tests are also given when first appear in a person who is over age 45 or who has other symptoms such as weight loss, because stomach cancer can cause similar symptoms . Also, when severe ulcers resist treatment, particularly if a person has several ulcers or the ulcers are in unusual places, a doctor may suspect an underlying condition that causes the stomach to overproduce acid.

Gastric ulcer
This endoscopic image shows a gastric ulcer, which upon biopsy was shown to be gastric cancer.
An esophagogastroduodenoscopy (EGD), a form of endoscopy, also known as a gastroscopy, is carried out on patients in whom a peptic ulcer is suspected. By direct visual identification, the location and severity of an ulcer can be described. Moreover, if no ulcer is present, EGD can often provide an alternative diagnosis.
If a peptic ulcer perforates, air will leak from the inside of the gastrointestinal tract (which always contains some air) to the peritoneal cavity (which normally never contains air). This leads to "free gas" within the peritoneal cavity. If the patient stands erect, as when having a chest x-ray, the gas will float to a position underneath the diaphragm. Therefore, gas in the peritoneal cavity, shown on an erect chest x-ray or supine lateral abdominal x-ray, is an omen of perforated peptic ulcer disease.
Treatment
Younger patients with ulcer-like symptoms are often treated with antacids.The ability of antacids to neutralize acidity by increasing the pH or blocking the secretion of acid by gastric cells is critical in reducing acidity in the stomach. Patients who are taking NSAIDs may also be prescribed a prostaglandin analogue in order to help prevent peptic ulcers by replacing the prostaglandins whose formation is blocked by NSAID use.
When H. pylori infection is present, the most effective treatments are combinations of two antibiotics, such as Clarithromycin, Amoxicillin, Tetracycline, and Metronidazole; and one proton pump inhibitor, sometimes in combination with antacids. In complicated, treatment-resistant cases, three antibiotics may be used together with a proton pump inhibitor. Treatment of H. pylori usually leads to clearing of infection, relief of symptoms and eventual healing of ulcers. Recurrence of infection can occur and retreatment may be required, if necessary with other antibiotics.
Perforated peptic ulcer is a surgical emergency and requires surgical repair of the perforation. Most bleeding ulcers require endoscopy urgently to stop bleeding with cautery, injection, or clipping.

Benign gastric ulcer
This gastric ulcer was found in tissue removed during a gastrectomy.