Most humans are not easily infected. Those who are weak, sick, malnourished, have cancer, or are diabetic have increased susceptibility to chronic or persistent infections. Individuals who have a suppressed immune system or who are on immunosuppressive drugs are particularly susceptible to opportunistic infections.
Risk of infection is a nursing diagnosis which is defined as "the state in which an individual is at risk to be invaded by an opportunistic or pathogenic agent (virus, fungus, bacteria, protozoa, or other parasite) from endogenous or exogenous sources. " The risk of infection depends on a number of endogenous sources. Skin damage from incision can increase a patient's risk of infection, as can very young or old age, due to a naive or compromised immune system respectively. Examples of risk factors include decreased immune system resulting from disease, compromised circulation caused by peripheral vascular disease, compromised skin integrity as a result of surgery, or repeated contact with contagious agents.
Risk Reduction
Techniques like hand washing, wearing gowns, and wearing face masks can help prevent infections from being passed between the surgeon and the patient. Frequent hand washing remains the most important defense against the spread of unwanted organisms. Good nutrition is necessary to reduce risk. So is a healthy lifestyle. By avoiding illicit drugs, using a condom, and entering an exercise program one can improve one's risk factors. Foods should be cooked to recommended temperatures; avoid foods that have been left outside for long. One should not take antibiotics for longer than needed or when they are not needed—long term use of antibiotics leads to resistance and increased the chance of developing opportunistic infections like clostridium difficile colitis . Vaccination is another vital means of preventing infections by encouraging the development of immune resistance in vaccinated hosts.
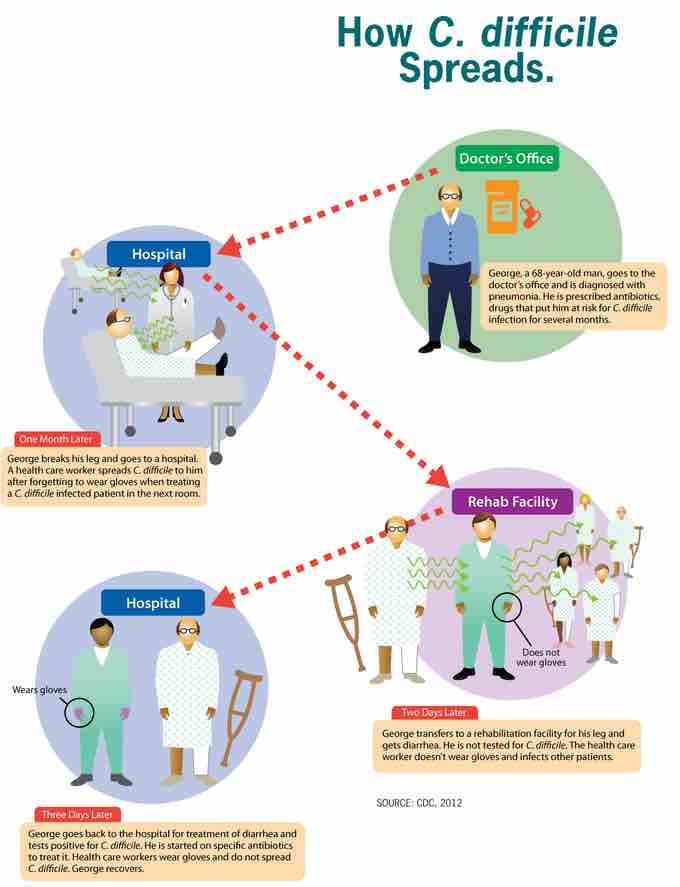
How C. difficile spreads
C. difficile is transmitted from person to person by the fecal-oral route. The organism forms large numbers of heat-resistant spores. These are not killed by alcohol-based hand cleansers or routine cleaning of surfaces. These spores remain viable in the hospital or nursing home environment for long periods of time. Because of this, the bacteria can be cultured from almost any surface in the hospital. Once spores are ingested by a patient, they pass through the stomach unscathed because of their acid-resistance. They germinate into vegetative cells in the colon upon exposure to bile acids, and multiply.