Technology: The Good
The use of advanced technology and molecular methods for detection, identification, and characterization of infectious agents is gaining importance in clinical microbiology laboratories. Emerging and re-emerging pathogens pose several challenges to diagnosis, treatment, and public health surveillance . Identification of an emerging pathogen by conventional methods is difficult and time-consuming due to the 'novel' nature of the agent. Identification requires a large array of techniques including cell cultures, inoculation of animals, cultivation using artificial media, histopathological evaluation of tissues (if available), and serological techniques using surrogate antigens.
Influenza
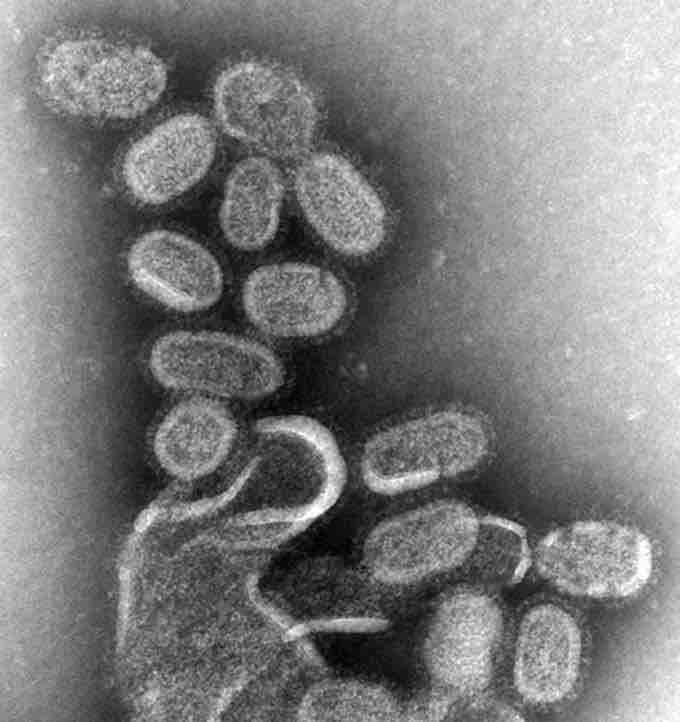
TEM of negatively stained influenza virions, magnified approximately 100,000 times. Modern transport contributes in spreading diseases faster.
Looking back at past epidemics or outbreaks caused by previously unknown infectious agents, we realize that identification and characterization of a new infectious agent can take years, decades, or even centuries. Such time frames have been decreased to weeks or months by the use of powerful molecular techniques, as seen with the identification of severe acute respiratory syndrome coronavirus (SARS-CoV) within weeks of the first cases reported, the discovery of a new hantavirus in North America in 1993, and the detection of bacteria as etiological pathogens of human infections such as Ehrlichia chaffeensis and Anaplasma phagocytophilum in human monocytotropic ehrlichiosis and human granulocytotropic anaplasmosis, respectively.
Molecular techniques offer several advantages over conventional methods, including high sensitivity and specificity, speed, ease of standardization, and automation. Other advantages include identification of novel, non-cultivable or very slowly growing organisms, strain typing in epidemiological studies, antimicrobial susceptibility determination, and monitoring treatment by measuring bacterial or viral loads.
Technology: The Bad
The effects of new technology on the environment are related to the emergence of many infectious diseases. For example, Lyme disease, hantavirus pulmonary syndrome (HPS), and Lassa fever all emerged when humans began encountering the insect vector (for Lyme disease) or rodent host (for HPS and Lassa fever) of the causative agents in greater numbers than ever before. Factors related to the emergence of infectious diseases such as Legionnaire disease and hemolytic uremic syndrome include changing technologies: air conditioning systems and mass food production, respectively.
Technology: The Ugly
Several human activities have led to the emergence and spread of new diseases:
ENCROACHMENT ON WILDLIFE HABITATS
The construction of new villages and housing developments in rural areas forces animals to live in dense populations, creating opportunities for microbes to mutate and emerge.
CHANGES IN AGRICULTURE
The introduction of new crops attracts new crop pests and the microbes they carry to farming communities, exposing people to unfamiliar diseases.
DESTRUCTION OF RAIN FORESTS
As countries make use of their rain forests by building roads and clearing areas for settlement or commercial ventures, people encounter insects and other animals harboring previously unknown microorganisms.
UNCONTROLLED URBANIZATION
The rapid growth of cities in many developing countries tends to concentrate large numbers of people into crowded areas with poor sanitation. These conditions foster transmission of contagious diseases.
MODERN TRANSPORT
Ships and other cargo carriers often harbor unintended 'passengers' that can spread diseases to faraway destinations. With international air travel, people infected with a disease can carry it to distant lands, or home to their families, before their first symptoms appear.