The skin flora, more properly referred to as the skin microbiome or skin microbiota, are the microorganisms that reside on the skin. Most bacteria on the skin are found in the superficial layers of the epidermis and the upper parts of hair follicles. Skin flora are usually non-pathogenic, and either commensals (are not harmful to their host) or mutualistic (offer a benefit). The benefits bacteria can offer include preventing transient pathogenic organisms from colonizing the skin surface, either by competing for nutrients, secreting chemicals against them, or stimulating the skin's immune system. However, resident microbes can cause skin diseases and enter the blood system creating life-threatening diseases particularly in immunosuppressed people. Hygiene to control such flora is important in preventing the transmission of antibiotic resistant hospital-acquired infections.
A major nonhuman skin flora is Batrachochytrium dendrobatidis, a chytrid and non-hyphal zoosporic fungus that causes chytridiomycosis, an infectious disease thought to be responsible for the decline in amphibian populations. The estimate of the number of species present on skin bacteria has been radically changed by the use of 16S ribosomal RNA to identify bacterial species present on skin samples direct from their genetic material. Previously such identification had depended upon microbiological culture upon which many varieties of bacteria did not grow and so were hidden to science. Staphylococcus epidermidis and Staphylococcus aureus were thought from cultural based research to be dominant. However, 16S ribosomal RNA research found that while common these species make up only 5% of skin bacteria. However, skin variety provides a rich and diverse habitat for bacteria. Most come from four phyla: Actinobacteria (51.8%), Firmicutes (24.4%), Proteobacteria (16.5%), and Bacteroidetes (6.3%).
There are three main ecological areas for skin flora: sebaceous, moist, and dry. Propionibacteria and Staphylococci species are the main species in sebaceous areas. In moist places on the body Corynebacteria together with Staphylococci dominate. In dry areas, there is a mixture of species, but b-Proteobacteria and Flavobacteriales are dominant. Ecologically, sebaceous areas have greater species richness than moist and dry ones. The areas with least similarity between people in species are the spaces between fingers, the spaces between toes, axillae, and umbilical cord stump. Most similar are beside the nostril, nares (inside the nostril), and on the back.
Skin microflora can be commensals, mutualistic, or pathogens. Often they can be all three depending upon the strength of the person's immune system. Research on the immune system in the gut and lungs has shown that microflora aids immunity development. However, such research has only started upon whether this is the case with the skin.
Pseudomonas aeruginosa is an example of a mutualistic bacterium that can turn into a pathogen and cause disease. If it gains entry into the blood system it can result in infections in bone, joint, gastrointestinal, and respiratory systems and it can also cause dermatitis. However, Pseudomonas aeruginosa produces antimicrobial substances such as pseudomonic acid (that are exploited commercially such as Mupirocin). This works against staphylococcal and streptococcal infections. Pseudomonas aeruginosa also produces substances that inhibit the growth of fungus species such as Candida krusei, Candida albicans, Torulopsis glabrata, Saccharomyces cerevisiae, and Aspergillus fumigatus. It can also inhibit the growth of Helicobacter pylori. Fatty acids (caproic acid) on the skin inhibit bacteria, especially after puberty, when undecylic acid becomes the primary fatty acid on the skin. Undecylic acid provides resistance to ringworm fungus and other skin infections.
Another aspect of bacteria is the generation of body odor. Sweat is odorless. However, several bacteria may consume it and create byproducts which may be considered putrid by man (as in contrast to flies, for example, that may find them attractive/appealing). For example, Propionibacteria in adolescent and adult produce propionic acid in sebaceous glands.
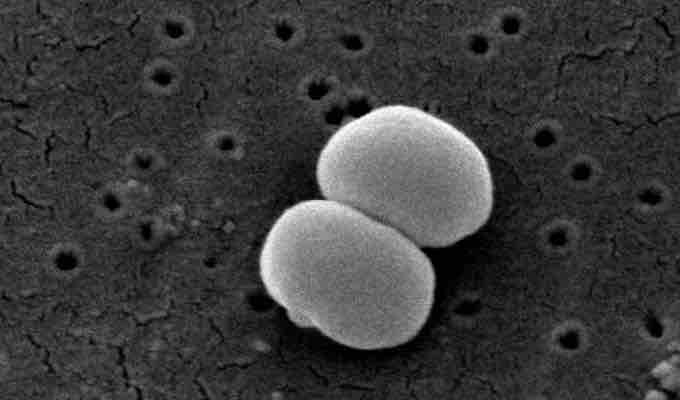
Staphylococcus epidermidis
Scanning electron microscope image of Staphylococcus epidermidis one of roughly 1,000 bacteria species present on human skin. Though usually not pathogenic, it can cause skin infections and even life threatening illnesses in those that are immunocompromised.