Blastomycosis (also known as "North American blastomycosis," "Blastomycetic dermatitis," and "Gilchrist's disease") is a fungal infection caused by the organism Blastomyces dermatitidis . Endemic to portions of North America, blastomycosis causes clinical symptoms similar to histoplasmosis.
Blastomycosis
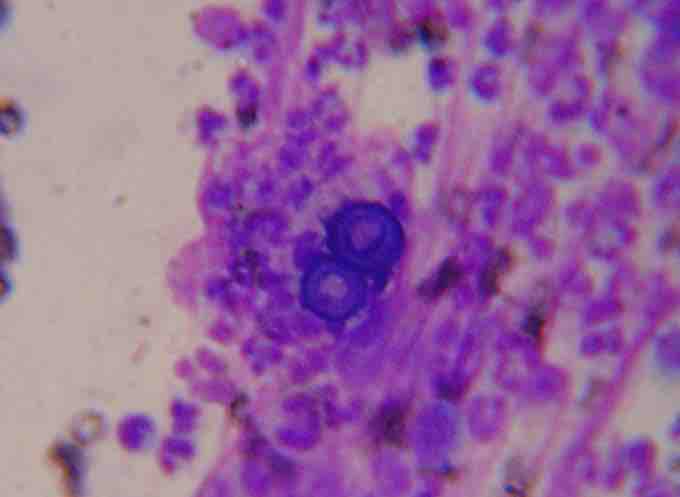
Blastomyces dermatitidis, the causative agent of blastomycosis.
Symptoms
Blastomycosis can present in one of the following ways:
- A flu-like illness with fever, chills, myalgia, headache, and a nonproductive cough which resolves within days
- An acute illness resembling bacterial pneumonia, with symptoms of high fever, chills, a productive cough, and pleuritic chest pain
- A chronic illness that mimics tuberculosis or lung cancer, with symptoms of low-grade fever, a productive cough, night sweats, and weight loss
- A fast, progressive, and severe disease that manifests as ARDS, with fever, shortness of breath, tachypnea, hypoxemia, and diffuse pulmonary infiltrates
- Skin lesions, usually asymptomatic, that appear as ulcerated lesions with small pustules at the margins
- Bone lytic lesions that can cause bone or joint pain.
- Prostatitis may be asymptomatic or may cause pain on urinating. Laryngeal involvement causes hoarseness.
Infection occurs by inhalation of the fungus from its natural soil habitat. Once inhaled in the lungs, Blastomycosis multiply and may disseminate through the blood and lymphatics to other organs, including the skin, bone, genitourinary tract, and brain. The incubation period is 30 to 100 days, although infection can be asymptomatic.
Diagnosis
Once suspected, the diagnosis of blastomycosis can usually be confirmed by demonstration of the characteristic, broad-based budding organisms in sputum or tissues by KOH prep, cytology, or histology. Tissue biopsy of skin or other organs may be required in order to diagnose extra-pulmonary disease. Blastomycosis is histologically associated with granulomatous nodules. Commercially available urine antigen testing appears to be quite sensitive in suggesting the diagnosis in cases where the organism is not readily detected. While culture of the organism remains the definitive diagnostic standard, its slow growing nature can lead to delays in treatment of up to several weeks.
Treatment
Itraconazole given orally is the treatment of choice for most forms of the disease. Ketoconazole may also be used. Cure rates are high, and the treatment over a period of months is usually well tolerated. Amphotericin B is considerably more toxic, and is usually reserved for immunocompromised patients who are critically ill and those with central nervous system disease. Fluconazole has also been tested on patients in Canada.