The humoral immune response (HIR) is the aspect of immunity mediated by secreted antibodies produced by B cells. Secreted antibodies bind to antigens on the surfaces of invading pathogens, which flag them for destruction. Humoral immunity is so named because it involves substances found in the humors, or body fluids. There are two types of humoral immunity: active and passive.
Active Humoral Immunity
Active humoral immunity refers to any form of immunity that occurs as a result of the formation of an adaptive immune response from the body's own immune system. Active immunity is long term (sometimes lifelong) because memory cells with antigen-binding affinity maturation are produced during the lymphocyte differentiation and proliferation that occurs during the formation of an adaptive immune response. It also refers to the effector functions of antibodies, which include pathogen and toxin neutralization, classical complement activation, and opsonin promotion of phagocytosis and pathogen elimination.
Active immunity can either be naturally-occurring or passive. Natural active immunity generally occurs as a result of infection with a pathogen, in which memory cells that remember the antigen of the infectious agent remain in the body. Artificial active immunity is the result of vaccination. During vaccination, the body is exposed to a weakened form of a pathogen that contains the same antigens as the live pathogen, but cannot mount an infection against the body in its weakened state. Vaccinations have become an effective form of disease prevention that is especially useful in preventing diseases that would normally have a high risk of mortality during an infection, where relying on natural active immunity would prove dangerous. However, active immunity does not work to protect against all pathogens, because many can mutate and change their antigen structure over time, which enables them to evade the defenses of immunological memory.
Passive Immunity
Passive immunity is the transfer of active humoral immunity in the form of ready-made antibodies from one individual to another. Passive immunization is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of ongoing or immunosuppressive diseases. Unlike active immunity, passive immunity is short-lived (often only for a few months), because it does not involve the production and upkeep of memory cells.
Passive immunity can occur naturally or artificially. Maternal passive immunity is a type of naturally-acquired passive immunity, and refers to antibody-mediated immunity conveyed to a fetus by its mother during pregnancy. IgG is passed through the placenta to the developing fetus, and is the only antibody isotype that can pass through the placenta. Because passive immunity is short-lived, vaccination is often required shortly following birth to prevent diseases such as tuberculosis, hepatitis B, polio, and pertussis; however, maternal antibodies can inhibit the induction of protective vaccine responses throughout the first year of life. This effect is usually overcome by secondary responses to booster immunization. Passive immunity is also provided through the transfer of IgA antibodies found in breast milk, which are transferred to the gastrointestinal tract of the infant, protecting against bacterial infections until the newborn has produced enough matured B cells to synthesize its own antibodies.
Artificially-acquired passive immunity is a short-term immunization achieved by the transfer of antibodies, and can be administered in several forms: as human or animal blood (usually horse) plasma or serum, as pooled human immunoglobulin for intravenous (IVIG) or intramuscular (IG) use, and as monoclonal antibodies (MAb). Passive transfer is used to help treat those with immunodeficiency and for several types of severe acute infections that have no vaccine, such as the Ebola virus. Immunity derived from passive immunization lasts for only a short period of time, and there is potential risk for hypersensitivity reactions and serum sickness, especially from gamma globulin of non-human origin. Passive immunity provides immediate protection, but the body does not develop memory; therefore, the patient is at risk of being infected by the same pathogen later.
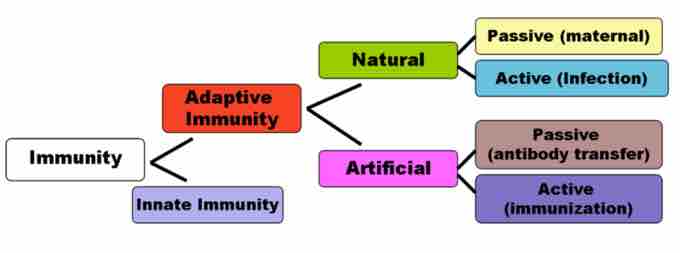
Innate and adaptive immunity in the immune system
This chart depicts the different divisions of immunity, including adaptive, innate, natural, artificial, passive (maternal), active (infection), passive (antibody transfer) and active (immunization).