Blood transfusions are a key therapeutic component to treating those with excessive blood loss from severe injury or surgery. Whole blood refers to blood drawn directly from the body from which none of the components, such as plasma or platelets, have been removed. The blood is typically combined with an anticoagulant during the collection process, but is otherwise unprocessed. Whole blood may also be altered and processed for use in blood transfusion.
Blood Processing
Historically, blood was transfused as whole blood without further processing. Most blood banks now split the whole blood into two or more components, typically red blood cells and a plasma component such as fresh frozen plasma, which is extracted frozen plasma from the blood splitting process.
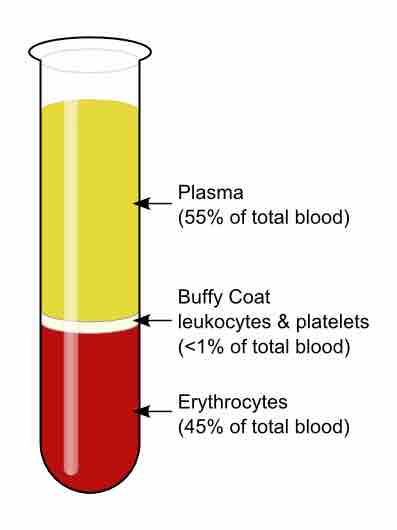
Platelets for transfusion can also be prepared from the buffy coat of whole blood, which has therapeutic benefits for those with platelet disorders or impaired clotting ability. Some blood banks have replaced this with platelets collected by plateletpheresis, a process in which platelets are extracted during initial blood collection. Plateletpheresis is more efficient because whole blood platelets typically aren't concentrated enough to have a useful effect, while plateletpheresis platelets are highly packed and concentrated. It also minimizes the chance for platelet transplant rejection because a single donor will be able to contribute enough platelets via plateletpheresis.
The collected blood is generally separated into components by one of three laboratory methods:
- Centrifuge quickly separates whole blood into plasma, buffy coat, and red cells by using centrifugal force to drop the cellular components to the bottom of a container.
- Sedimentation, in which whole blood sits overnight, causing the red blood cells and plasma to settle and slowly separate by the force of normal gravity.
Practical Considerations
Whole blood transfusion has similar risks to those of transfusion of red blood cells. It must be cross-matched on the basis of blood type to avoid hemolytic transfusion reactions. Most of the indications for use are identical to those for red blood cells. Whole blood is not used because the extra plasma can contribute to transfusion associated circulatory overload (TACO), a potential complication that can dangerously increase blood pressure, causing pulmonary edema and acute respiratory distress.
Whole blood is sometimes "recreated" from stored red blood cells and fresh frozen plasma for neonatal transfusions. This provides a final product with a very specific hematocrit (percentage of red cells) with type O red cells and type AB plasma to minimize the chance of complications.
Whole blood is typically stored under the same conditions as red blood cells and can be kept up to 35 days if collected with CPDA-1 storage solution or 21 days with other common storage solutions such as CPD. If the blood will be used to make platelets, it is kept at room temperature until the process is complete. This must be done quickly to minimize the warm storage of RBCs in the unit.
Centrifuged Blood
Whole blood is a term used in transfusion medicine for human blood from a standard blood donation.

Blood Transfusions
Blood transfusions are common during surgeries.