Fibrinolysis is a process that removes clots following hemostasis and clot retraction, preventing uncontrolled thrombosis and embolism. There are two types of fibrinolysis: primary fibrinolysis and secondary fibrinolysis. Primary fibrinolysis is a normal body process, whereas secondary fibrinolysis is the breakdown of clots due to a medication, medical disorder, or other cause.
Mechanisms of Primary Fibrinolysis
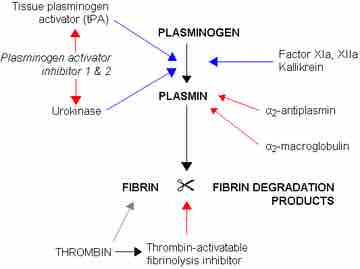
Primary fibrinolysis normally occurs following clot retraction, in which the clot has already condensed considerably in size. The main enzyme in primary fibrinolysis is plasmin, a proteolytic enzyme that degrades fibrin mesh. Plasmin cleaves fibrin at various places, leading to the production of circulating fragments that are cleared by other proteases or by the kidneys and liver.
Plasmin is produced in an inactive form, plasminogen, in the liver. Plasminogen cannot cleave fibrin and circulates in the bloodstream. Instead, it is incorporated into the clot when it is formed and then activated into plasmin later. Plasminogen is activated to plasmin by tissue plasminogen activator (t-PA) and urokinase, an enzyme found in the urine.
Fibrinolysis
Blue arrows denote stimulation and red arrows inhibition.
T-PA is released into the blood very slowly by the damaged endothelium of the blood vessels. T-PA and urokinase are themselves inhibited by plasminogen activator inhibitor-1 and plasminogen activator inhibitor-2 (PAI-1 and PAI-2). In contrast, plasmin further stimulates plasmin generation by producing more active forms of both tissue plasminogen activator (tPA) and urokinase. Following fibrin degradation by plasmin, old activated platelets from the platelet plug are phagocytized and destroyed by macrophages.
Alpha 2-antiplasmin and alpha 2-macroglobulin inactivate plasmin. Plasmin activity is also reduced by thrombin-activatable fibrinolysis inhibitor (TAFI), which modifies fibrin to make it more resistant to the tPA-mediated plasminogen. Plasmin operates on a negative feedback process because it is reduced when the fibrin clot is fully degraded.
Mechanisms of Secondary Fibrinolysis
Secondary fibrinolysis generally refers to treatment of pathological thromboembolism. If blood clots embolize to different parts of the body, they can cause tissue death by blocking off blood flow to those tissues. This is a common cause of heart attacks, pulmonary embolism, and strokes. Several medications exist to help treat and prevent these conditions.
Fibrinolytic drugs include synthesized tissue plasminogen activator and streptokinase, a bacterial enzyme that has degrades fibrin directly. Clots may also be prevented or kept from worsening through the use of blood thinners (anticoagulants). Aspirin has anticoagulant properties because it inhibits cyoclo-oxygenase dependent pathways of platelet activation, which can prevent clotting from worsening. Heparin is a fast-acting anticoagulant produced by the body and used as a drug which inhibits the activity of thrombin. Warfarin inhibits vitamin K cofactor activation during the coagulation cascade, and citrates chelate calcium to prevent prothrombin activation into thrombin.
All of these treatments have been shown to have tremendous therapeutic benefit in treating those with thromboembolic diseases; however, they can make injury much more difficult to treat by disrupting the clotting process. For example, patients thought to be suffering from a stroke (obstructed artery in the brain) must be screened through imaging before given aspirin or a fibrinolytic drug, because if they have an aneurysm or hemorrhage (burst blood vessel or bleeding in the brain), administering fibrinolytic treatment would make their condition worse and possibly fatal by inhibiting the clotting that could save their lives.