Peritonitis is an inflammation of the peritoneum , the thin tissue that lines the inner wall of the abdomen and covers most of the abdominal organs. Peritonitis may be localized or generalized, and may result from infection (often due to rupture of a hollow organ as may occur in abdominal trauma or appendicitis) or from a non-infectious process.
Peritoneum
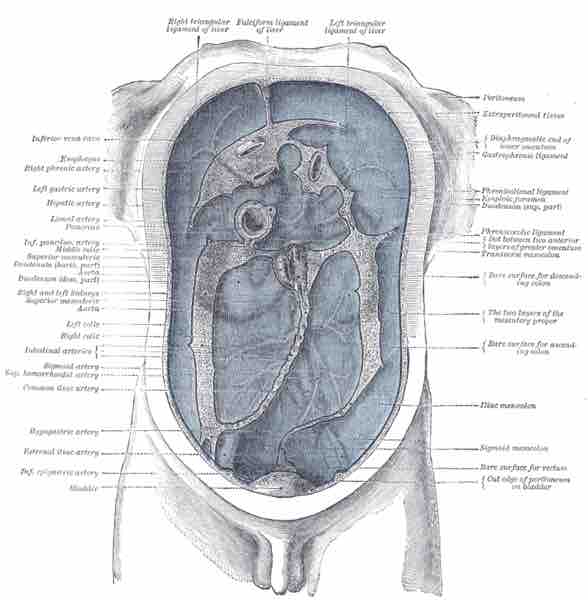
The peritoneum, colored in blue, is the serous membrane that forms the lining of the abdominal cavity. It covers most of the intra-abdominal, supporting them and serving as a conduit for their blood and lymph vessels and nerves. Peritonitis is an inflammation of the peritoneum often causing abdominal pain and tenderness.
The main manifestations of peritonitis are acute abdominal pain, abdominal tenderness, and abdominal guarding, which are exacerbated by moving the peritoneum by coughing, flexing one's hips, or eliciting the Blumberg sign. Diffuse abdominal rigidity ("washboard abdomen") is often present, especially in generalized peritonitis. Other symptoms include fever, sinus tachycardia, and development of intestinal paralysis, which also causes nausea, vomiting, and bloating.
Complications of peritonitis include sequestration of fluid and electrolytes, as revealed by decreased central venous pressure, which may cause electrolyte disturbances, as well as significant hypovolemia, possibly leading to shock and acute renal failure. A peritoneal abscess may form and sepsis may develop, so blood cultures should be obtained.
Perforation of part of the gastrointestinal tract is the most common cause of peritonitis. Examples include perforation of the distal esophagus, of the stomach by a peptic ulcer or gastric carcinoma, of the duodenum, of the remaining intestine by appendicitis, diverticulitis, inflammatory bowel disease (IBD), intestinal infarction, intestinal strangulation, colorectal carcinoma, or of the gallbladder. Other possible reasons for perforation include abdominal trauma, ingestion of a sharp foreign body (such as a fish bone, toothpick or glass shard), perforation by an endoscope or catheter, and internal leakage of a colostomy site. In most cases of perforation of a hollow viscus, mixed bacteria are isolated from the infection; the most common agents include Gram-negative bacilli like E. coli and anaerobic bacteria. Fecal peritonitis results from the presence of feces in the peritoneal cavity. It can result from abdominal trauma and occurs if the large bowel is perforated during surgery.
Disruption of the peritoneum, even in the absence of perforation of a hollow viscus, may also cause infection simply by letting micro-organisms into the peritoneal cavity. Examples include trauma, surgical wound, continuous ambulatory peritoneal dialysis, and intra-peritoneal chemotherapy. Again, in most cases, mixed bacteria are isolated; the most common agents include cutaneous species such as Staphylococcus aureus, and coagulase-negative staphylococci, but many others are possible, including fungi such as Candida.
Spontaneous bacterial peritonitis (SBP) is a peculiar form of peritonitis occurring in the absence of an obvious source of contamination. It occurs in patients with excess fluid in their abdomens, particularly in children. Intra-peritoneal dialysis predisposes a patient to peritoneal infection. Systemic infections such as tuberculosis may rarely have a peritoneal localization.
Sterile abdominal surgery, under normal circumstances, causes localized or minimal generalized peritonitis. However, peritonitis may also be caused by the rare case of a sterile foreign body inadvertently left in the abdomen after surgery (e.g., gauze, sponge). Much rarer non-infectious causes may include familial Mediterranean fever, porphyria, and systemic lupus erythematosus.
Depending on the severity of the patient's state, the management of peritonitis may include supportive measures, antibiotics, or surgery. General supportive measures include vigorous intravenous rehydration and correction of electrolyte disturbances. Antibiotics are usually administered intravenously, but they may also be infused directly into the peritoneum. The empiric choice of broad-spectrum antibiotics often consist of multiple drugs, and should be targeted against the most likely agents, depending on the cause of peritonitis; once one or more agents are actually isolated, therapy will of course be targeted on them. Surgery is needed to perform a full exploration and lavage of the peritoneum, as well as to correct any gross anatomical damage that may have caused peritonitis. The exception is spontaneous bacterial peritonitis, which does not always benefit from surgery and may be treated with antibiotics in the first instance.
If properly treated, typical cases of surgically correctable peritonitis (e.g., perforated peptic ulcer, appendicitis, and diverticulitis) have a mortality rate of <10% in otherwise healthy patients, which rises to about 40% in the elderly, and/or in those with significant underlying illness, as well as in cases that present late (after 48 hours). If untreated, generalized peritonitis is almost always fatal.