Cornea
Background to the schools Wikipedia
SOS Children offer a complete download of this selection for schools for use on schools intranets. A quick link for child sponsorship is http://www.sponsor-a-child.org.uk/
| Cornea | |
|---|---|
 |
|
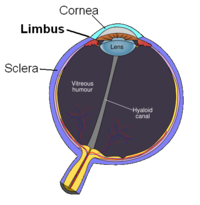
| Schematic diagram of the human eye. (Cornea labeled at centre top.) | |
 |
|
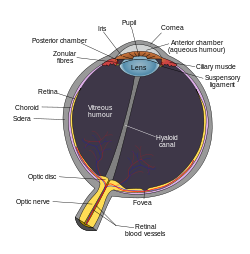
| Vertical section of human cornea from near the margin. (Waldeyer.) Magnified. 1. Epithelium. 2. Anterior elastic lamina. 3. substantia propria. 4. Posterior elastic lamina. 5. Endothelium of the anterior chamber. a. Oblique fibers in the anterior layer of the substantia propria. b. Lamellæ the fibers of which are cut across, producing a dotted appearance. c. Corneal corpuscles appearing fusiform in section. d. Lamellæ the fibers of which are cut longitudinally. e. Transition to the sclera, with ass more distinct fibrillation, and surmounted by a thicker epithelium. f. Small bloodvessels cut across near the margin of the cornea. |
|
| Gray's | subject #225 1006 |
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Together with the lens, the cornea refracts light, and as a result helps the eye to focus, accounting for approximately 80% of the eye's optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. While the cornea contributes most of the eye's focusing power, its focus is fixed. The curvature of the lens, on the other hand, can be adjusted to "tune" the focus depending upon the object's distance. Medical terms related to the cornea often start with the prefix " kerat-".
Structure
The cornea has unmyelinated nerve endings sensitive to touch, temperature and chemicals; a touch of the cornea causes an involuntary reflex to close the eyelid. Because transparency is of prime importance the cornea does not have blood vessels; it receives nutrients via diffusion from the tear fluid at the outside and the aqueous humour at the inside and also from neurotrophins supplied by nerve fibres that innervate it. In humans, the cornea has a diameter of about 11.5 mm and a thickness of 0.5–0.6 mm in the centre and 0.6–0.8 mm at the periphery. Transparency, avascularity, and immunologic privilege makes the cornea a very special tissue. The cornea is the only part of a human body that has no blood supply; it gets oxygen directly through the air.
It borders with the sclera by the corneal limbus.
Layers
The human cornea, like that of other primates, has five layers. The corneas of cats, dogs, and other carnivores have only four. From the anterior to posterior they are:
- Corneal epithelium: a thin epithelial multicellular tissue layer (stratified squamous epithelium) of fast-growing and easily-regenerated cells, kept moist with tears. Irregularity or edema of the corneal epithelium disrupts the smoothness of the air-tear film interface, the most significant component of the total refractive power of the eye, thereby reducing visual acuity.
- Bowman's layer (also erroneously known as the anterior limiting membrane, when in fact it is not a membrane but a condensed layer of collagen): a tough layer that protects the corneal stroma, consisting of irregularly-arranged collagen fibers. This layer is absent in carnivores.
- Corneal stroma (also substantia propria): a thick, transparent middle layer, consisting of regularly-arranged collagen fibers along with sparsely populated keratocytes. The corneal stroma consists of approximately 200 layers of type I collagen fibrils. There are 2 theories of how transparency in the cornea comes about:
- The lattice arrangements of the collagen fibrils in the stroma. The light scatter by individual fibrils is cancelled by destructive interference from the scattered light from other individual fibrils.(Maurice)
- The spacing of the neighbouring collagen fibrils in the stroma must be < 200 nm for there to be transparency. (Goldman and Benedek)
- Descemet's membrane (also posterior limiting membrane): a thin acellular layer that serves as the modified basement membrane of the corneal endothelium.
- Corneal endothelium: a simple squamous or low cuboidal monolayer of mitochondria-rich cells responsible for regulating fluid and solute transport between the aqueous and corneal stromal compartments. (The term endothelium is a misnomer here. The corneal endothelium is bathed by aqueous humour, not by blood or lymph, and has a very different origin, function, and appearance from vascular endothelia.)
Innervation
The cornea is one of the most sensitive tissues of the body, it is densely innervated with sensory nerve fibres via the ophthalmic division of the trigeminal nerve by way of 70 - 80 long ciliary nerves; and short ciliary nerves derived from the oculomotor nerve.
The nerves enter the cornea via three levels, scleral, episcleral and conjunctival. Most of the bundles give rise by subdivision to a network in the stroma, from which fibres supply the different regions. The three networks are midstromal, subepithelial/Bowman's layer, and epithelium. The receptive fields of each nerve ending are very large, and may overlap.
Corneal nerves of the subepithelial layer converge and terminate near the apex of the cornea in a logarithmic spiral pattern.
Diseases and disorders
Treatment and management
Surgical procedures
Various refractive eye surgery techniques change the shape of the cornea in order to reduce the need for corrective lenses or otherwise improve the refractive state of the eye. In many of the techniques used today, reshaping of the cornea is performed by photoablation using the excimer laser.
If the corneal stroma develops visually significant opacity, irregularity, or edema, a cornea of a deceased donor can be transplanted. Because there are no blood vessels in the cornea, there are also few problems with rejection of the new cornea.
There are also synthetic corneas (keratoprostheses) in development. Most are merely plastic inserts, but there are also composed of biocompatible synthetic materials that encourage tissue ingrowth into the synthetic cornea, thereby promoting biointegration.
Non-surgical procedures
Orthokeratology is a method using specialized hard or rigid gas-permeable contact lenses to transiently reshape the cornea in order to improve the refractive state of the eye or reduce the need for eyeglasses and contact lenses.