A person's social class has a significant impact on their physical health, their ability to receive adequate medical care and nutrition, and their life expectancy. While gender and race play significant roles in explaining healthcare inequality in the United States, socioeconomic status (SES) is the greatest social determinant of an individual's health outcome. Social determinants of health are the economic and social conditions that influence individual and group differences in health status. Social determinants are environmental, meaning that they are risk factors found in one's living and working conditions (including the distribution of income, wealth, influence, and power), rather than individual factors (such as behavioral risk factors or genetics). Social determinants can be used to predict one's risk of contracting a disease or sustaining an injury, and can also indicate how vulnerable one is to the consequences of a disease or injury. Individuals of lower socioeconomic status have lower levels of overall health, less insurance coverage, and less access to adequate healthcare than those of higher SES.
Individuals with a low SES in the United States experience a wide array of health problems as a result of their economic position. They are unable to use healthcare as often as people of higher status and when they do, it is often of lower quality. Additionally, people with low SES tend to experience a much higher rate of health issues than those of high SES. Many social scientists hypothesize that the higher rate of illness among those with low SES can be attributed to environmental hazards. For example, poorer neighborhoods tend to have fewer grocery stores and more fast food chains than wealthier neighborhoods, increasing nutrition problems and the risk of conditions, such as heart disease. Similarly, poorer neighborhoods tend to have fewer recreational facilities and higher crime rates than wealthier ones, which decreases the feasibility of routine exercise.
In addition to having an increased level of illness, lower socioeconomic classes have lower levels of health insurance than the upper class. Much of this disparity can be explained by the tendency for middle and upper class people to work in professions that provide health insurance benefits to employees, while lower status occupations often do not provide benefits to employees. For many employees who do not have health insurance benefits through their job, the cost of insurance can be prohibitive. Without insurance, or with inadequate insurance, the cost of healthcare can be extremely high. Consequently, many uninsured or poorly insured individuals do not have access to preventative care or quality treatment. This group of people has higher rates of infant mortality, cancer, cardiovascular disease, and disabling physical injuries than are seen among the well insured.
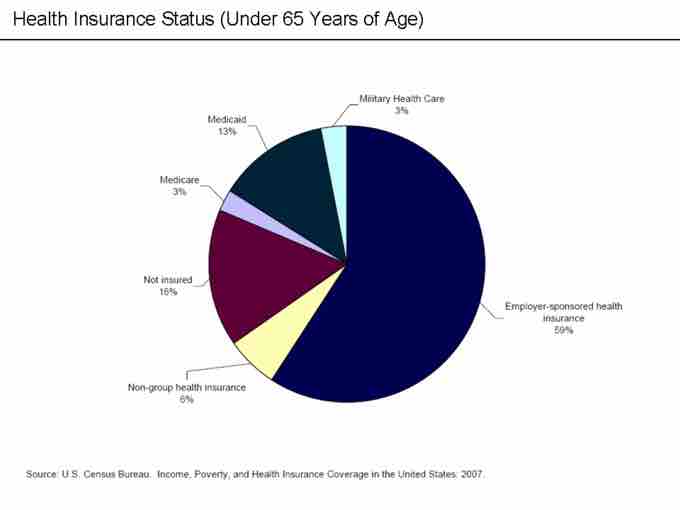
Health Insurance Distribution (under 65 years)
As seen in this graph, with insurance needed for most health services, access to healthcare is not evenly distributed among Americans. The largest group of insured Americans consists of middle and upper class employees who receive health insurance through employers. As of 2007, 16% of the population had no health insurance coverage and, thus, had greatly limited access to healthcare.
Health inequality refers to the unequal distribution of environmental health hazards and access to health services between demographic groups, including social classes. For example, poor and affluent urban communities in the United States are geographically close to each other and to hospitals. Still, the affluent communities are more likely to have access to fresh produce, recreational facilities for exercise, preventative healthcare programs, and routine medical visits. Consequently, affluent communities are likely to have better health outcomes than nearby impoverished ones. The role of socioeconomic status in determining access to healthcare results in heath inequality between the upper, middle, and lower or working classes, with the higher classes having more positive health outcomes.

Farmers Market
Farmers markets are visible sources of fresh produce and healthy foods. These markets are concentrated in middle to upper income neighborhoods and are not found in food deserts.