Background
In March 2010, President Obama gave a speech at a rally in Pennsylvania explaining the necessity of health insurance reform. The speech called on Congress to hold a final up or down vote on reform. As of 2012, the legislation remains controversial, with some states challenging it in federal court. There has also been opposition from some voters. In June 2012, in a 5–4 decision, the U.S. Supreme Court found the law to be constitutional.
Expanding Medicaid and Subsidizing Insurance
The law includes health-related provisions that take effect over several years. The law intends to expand Medicaid eligibility for people making up to 133% of the federal poverty level (FPL). It would subsidize insurance premiums for people making up to 400% of the FPL ($88,000 for family of 4 in 2010) so their maximum "out-of-pocket" payment for annual premiums would be on sliding scale from 2% to 9.5% of income. The law also intends to provide incentives for businesses to offer health care benefits, prohibit denial of coverage and denial of claims based on pre-existing conditions, establish health insurance exchanges, prohibit insurers from establishing annual coverage caps, and provide support for medical research.
Guaranteed Issue, Community Rating, Individual Mandate
Starting in 2014, the law will prohibit insurers from denying coverage (see guaranteed issue) to sicker applicants or imposing special conditions such as higher premiums or payments (see community rating). Health care expenditures are highly concentrated with the most expensive 5% of the population accounting for half of aggregate health care spending. The bottom 50% of spenders account for only 3% of health care spending. This means that what insurance companies gain from avoiding the sick greatly outweighs any possible gains from managing their care. As a result, insurers devoted resources to such avoidance at a direct cost to effective care management, which is against the interests of the insured. Instead of providing health security, the health insurance industry had, since the 1970's, begun to compete by becoming risk differentiators. They sought to only insure people with good or normal health profiles and exclude those considered to be or likely to become unhealthy and therefore less profitable. According to a study from Cambridge Hospital, Harvard Law School, and Ohio University, 62% of all 2007 personal bankruptcies in the United States were driven by medical incidents, with (75% having had) health insurance.
Also beginning in 2014, the law will generally require uninsured individuals to buy government-approved health insurance — the individual mandate. Government-run exchanges may present information to facilitate comparison among competing plans, if available, but previous attempts at creating similar exchanges only produced mixed results. This requirement is expected to reduce the number of the uninsured from 19% of all residents in 2010 to 8% by 2016. Some analysts believe that the 8% figure of uninsured are expected to be mostly illegal immigrants (5%), with the rest paying the fine unless exempted. Whether or not this is true remains unclear based on the present available data.
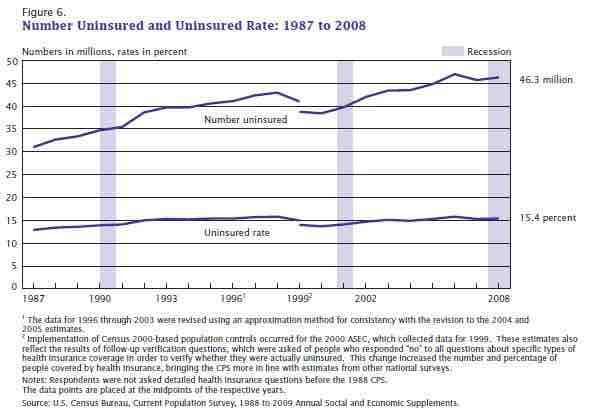
Uninsured and Uninsured Rate (1987 to 2008)
This image depicts the number of uninsured Americans and the uninsured rate from 1987 to 2008.
Some analysts have argued that the insurance premium structure may shift more costs onto younger and healthier people. Approximately $43 billion was spent in 2008 providing non-reimbursed emergency services for the uninsured, which the Act's supporters argued increased the average family's insurance premiums. Other studies claim the opposite that the argument for reduced ER visits has been shown to be largely a canard [...] insuring the uninsured will lead to, very approximately, a doubling of health expenditures for the currently uninsured. The studies suggest that making insurance mandatory rather than voluntary will tend to bring younger, healthier people into the insurance pool, shifting the cost of the Act's increased spending onto them.