Transfusion medicine is extremely effective at treating those with severe blood loss. Transfusions are often a required component of major surgeries. Due to the different antigen blood types, blood must be cross-matched during processing to avoid potential complications.
The Cross-Matching Process
Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every recipient is given blood that is compatible and is as safe as possible. Several laboratory tests allow cross-matching of compatible blood between donor and recipient. Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. Risks can be further reduced by cross-matching blood, but this process isn't always performed if time is short and the need for transfusion has not been anticipated.
Cross-matching involves mixing a sample of the recipient's serum with a sample of the donor's red blood cells and checking if the mixture agglutinates, or forms clumps. These clumps are the result of antibodies binding the red blood cells together. If agglutination is not obvious by direct vision, blood bank technicians check for agglutination with a microscope. If agglutination occurs, that particular donor's blood cannot be transfused to that particular recipient. In a blood bank, it is vital that all blood specimens are correctly identified, so labeling has been standardized using a barcode system known as ISBT 128. The blood group may be included on identification by military personnel in case they need an emergency blood transfusion.
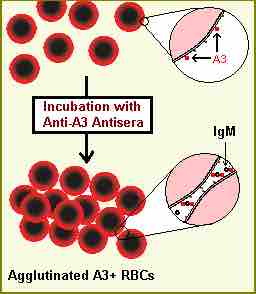
Agglutinated RBC
Red blood cells can agglutinate if the serum contains antibodies against the expressed proteins. In this image, the blood serum contains anti-A3 antibodies, which attack and agglutinate type A blood.
Potential Transfusion Complications
If a patient receives blood during a transfusion that is not compatible with his or her blood type, severe problems can occur. Acute hemolytic transfusion reactions occur if donated blood cells are attacked by matching host antibodies. This can cause shock-like symptoms, such as fever, hypotension, and disseminated intravascular coagulation from immune system mediated endothelial damage. Transfusion reactions are also associated with acute renal failure. Lung injury is common as well, due to pulmonary edema from fluid overload if plasma volume becomes too high or neutrophil activation during a transfusion reaction. If the donated blood is contaminated with bacteria, it may induce septic shock in the patient.