The second critical step in hemostasis, which follows vasoconstriction, is platelet plug formation. The three steps to platelet plug formation are platelet adherence, activation, and aggregation.
Platelet Adherence
Normally, the endothelial cells express molecules that inhibit platelet adherence and activation while platelets circulate through the blood vessels. These molecules include nitric oxide, prostacylcine (PGI2) and endothelial ADP-ase.
During an injury, subendothelial collagen from the extracellular matrix beneath the endothelial cells is exposed on the epithelium as the normal epithelial cells are damaged and removed, which releases von Willebrand Factor (VWF). VWF causes the platelets to change form with adhesive filaments (extensions) that adhere to the subendothelial collagen on the endothelial wall.
Platelet Activation
After platelet adherence occurs, the subendothelial collagen binds to receptors on the platelet, which activates it. During platelet activation, the platelet releases a number of important cytokines and chemical mediators via degranulation. The released chemicals include ADP, VWF, thromboxane A2, platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), serotonin, and coagulation factors. The extra ADP and VWF is especially important because it causes nearby platelets to adhere and activate, as well as release more ADP, VWF, and other chemicals. Platelet plug formation is considered a positive feedback process because ADP and VWF levels are successively increased as more and more platelets activate to form the plug.
The other factors released during platelet activation perform other important functions. Thromboxane is an arachidonic acid derivative (similar to prostaglandins) that activates other platelets and maintains vasoconstriction. Serotonin is a short-lived inflammatory mediator with a vasoconstrictive effect that contributes to vascular changes associated with inflammation during an injury. PDGF and VEGF are involved in angiogenesis, the growth of new blood vessels and cell cycle proliferation (division) following injury. The coagulation factors include factor V and VIII, which are involved in the coagulation cascade that converts fibrinogen into fibrin mesh after platelet plug formation.
Platelet Aggregation
The final step of platelet plug formation is aggregation of the platelets into a barrier-like plug. Receptors on the platelet bind to VWF and fibrinogen molecules, which hold the platelets together. Platelets may also bind to subendothelial VWF to anchor them to the damaged endothelium. The completed plug will cover the damaged components of the endothelium and will stop blood from flowing out of it, but if the wound is large enough, blood will not coagulate until the fibrin mesh from the coagulation cascade is produced, which strengthens the platelet plug. If the wound is minor, the platelet plug may be enough to stop the bleeding without the coagulation cascade.
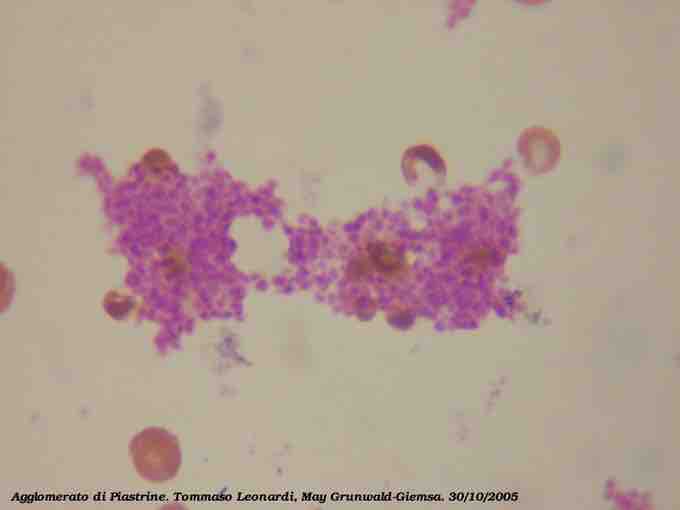
Platelets
A blood slide of platelets aggregating or clumping together. The platelets are small, bright purple fragments.
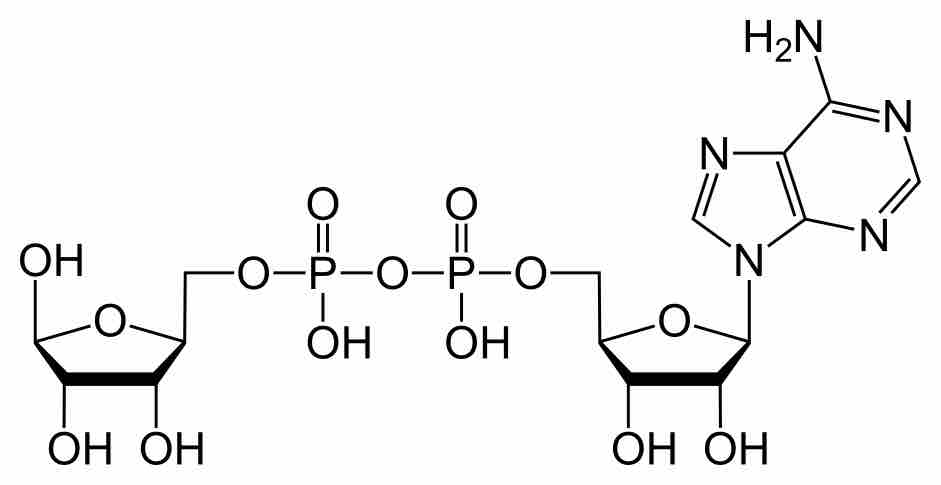
ADP
The chemical structure of ADP, a molecule that causes platelet activation and is involved in the positive feedback component of platelet activation.