Fluid can leave the body in several ways: urination, excretion (feces), and perspiration (sweating). The majority of fluid output occurs via the urine, at approximately 1500 ml/day (approx 1.59 qt/day) in a normal adult at resting state. Some fluid is lost through perspiration (part of the body's temperature control mechanism) and as water vapor in expired air, however these fluid losses are considered to be very minor.
The body's homeostatic control mechanisms, which maintain a constant internal environment, ensure that a balance between fluid gain and fluid loss is maintained. The hormones ADH (anti-diuretic hormone, also known as vasopressin) and aldosterone, a hormone created by the renin-angiotensin system play a major role in this. If the body is becoming fluid-deficient, there will be an increase in the secretion of these hormones, causing water to be retained by the kidneys through increased tubular reabsorption and urine output to be reduced. Conversely, if fluid levels are excessive, secretion of these hormones is suppressed, resulting in less retention of fluid by the kidneys and a subsequent increase in the volume of urine produced, due to reduced fluid retention.
ADH Feedback
When blood volume becomes too low, plasma osmolarity will increase due to a higher concentration of solutes per volume of water. Osmoreceptors in the hypothalamus detect the increased plasma osmolarity and stimulate the posterior pituitary gland to secrete ADH, which is also known as vasopressin. ADH causes the walls of the distal convoluted tubule and collecting duct to become permeable to water, drastically increasing the amount of water that is reabsorbed during tubular reabsorption. ADH also has a vasoconstrictive effect in the cardiovascular system, which makes it one of the most important compensatory mechanisms during hypovolemic shock (shock from excessive fluid loss or bleeding).
Aldosterone Feedback
Aldosterone is a steroid hormone (corticoid) produced at the end of the renin-angiotensin system. To review the renin-angiotensin system, low blood volume activates the juxtaglomerular apparatus in a variety of ways, which secretes renin. Renin cleaves angiotensin I from the liver produced angiotensinogen. Angiotensin converting enzyme (ACE) in the lungs converts angiotensin I into angiotensin II. Angiotensin II has a variety of effects (such as increasing thirst) but it also causes release of aldosterone from the adrenal cortex.
Aldosterone has a number of effects involved in the regulation of water output. It acts on mineralcorticoid receptors in the epithelial cells of the distal convoluted tubule and collecting duct, which increases their expression of Na+/K+ ATPase pumps and activates those pumps. This causes greatly increased reabsorption of sodium and water (which follows sodium osmotically by cotransport) while causing the secretion of potassium into urine. Aldosterone therefore increases water reabsorption, however it involves an exchange of sodium and potassium, which ADH reabsoption regulation does not involve. Aldosterone will also cause a similar ion balancing effect in the colon and salivary glands as well.
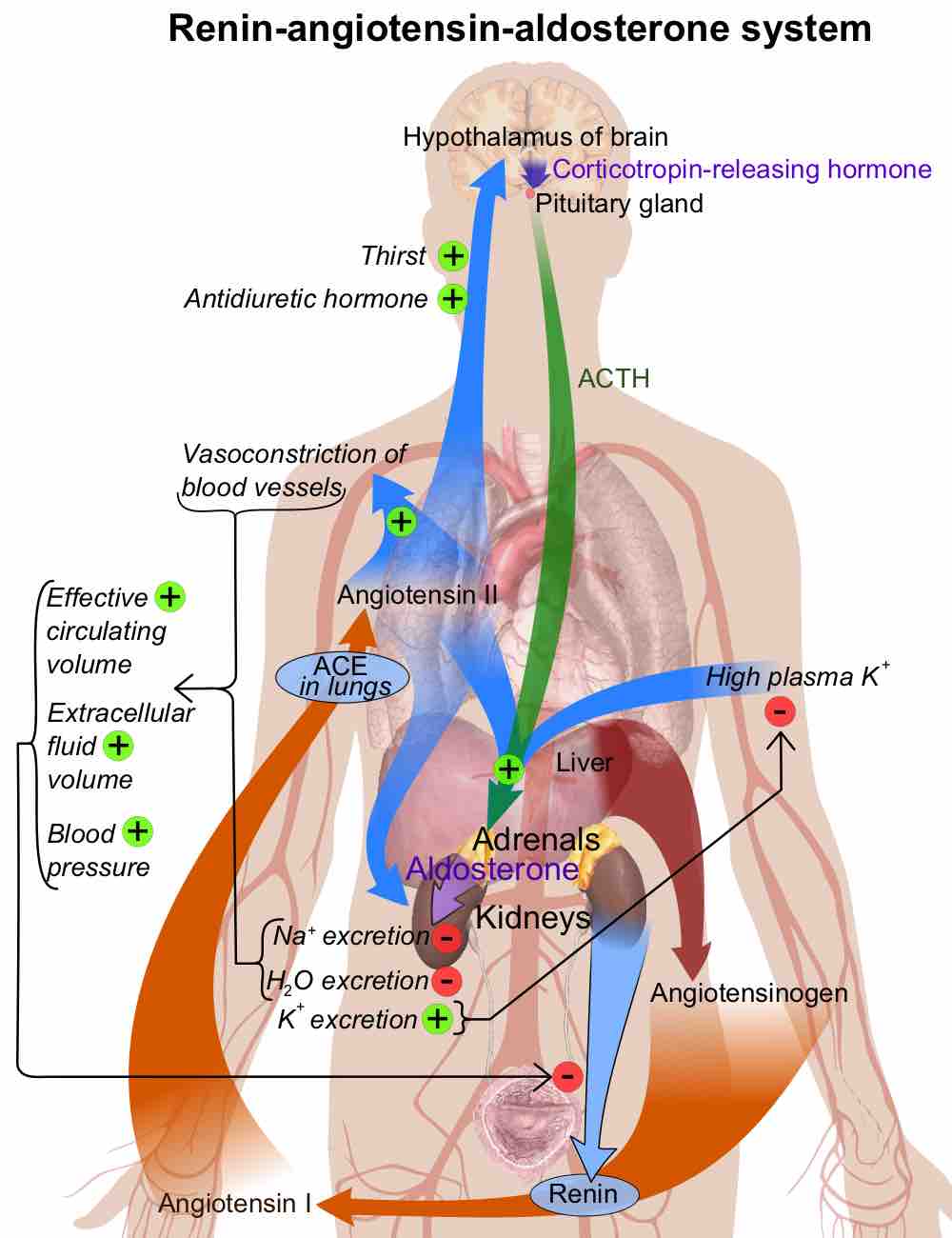
Schematic diagram of renin–angiotensin–aldosterone system
Overview of the renin-angiotensin system that regulates blood pressure and plasma osmolarity.