Global CV changes with aging
The heart muscle becomes less efficient with age, and there is a decrease in both maximum cardiac output and heart rate, although resting levels may be more than adequate.
The health of the myocardium depends on its blood supply, and with age there is greater likelihood that arthrosclerosis will narrow the coronary arteries. The heart loses about one percent of its reserve plumbing capacity every year after we turn 30. Changes in blood vessels that serve brain tissue reduce nourishment to the brain, resulting in the malfunction and death of brain cells. By the time we turn 80, cerebral blood flow is 20% less, and renal blood flow is 50% less than when we were age 30. As we age, our heart goes through certain structural changes: the walls of the heart thicken and the heart becomes heavier; heart valves stiffen and are more likely to calcify; and the aorta, the major vessel carrying blood out of the heart, becomes larger.
INFARCT DEVELOPMENT
High blood pressure (hypertension) causes the left ventricle to work harder. The ventricle muscle may enlarge and outgrow its blood supply, thus becoming weaker. A weak ventricle is not an efficient pump, and may progress to congestive heart failure. This process may be slow or rapid. Acute myocardial infarction (AMI or MI), commonly known as a heart attack, is a disease that occurs when the blood supply to a part of the heart is interrupted, causing death of heart tissue.
Athersclerosis can lead to an MI. It is the leading cause of death for both men and women all over the world. The term myocardial infarction is derived from myocardium (the heart muscle) and infarction (tissue death). Atherosclerosis is the deposition of cholesterol on and in the walls of the arteries, which narrows the lumen, decreases blood flow, and forms rough surfaces that may cause intravascular clot formation .
The phrase "heart attack" sometimes refers to heart problems other than MI, such as unstable angina pectoris and sudden cardiac death. With aging, the integrity of the endothelium, lining the blood vessels and coronary arteries, is reduced and the likelihood of plaque formation and infarct development is increased.
ARRHYTHMIAS AND FIBROSIS
Arrhythmias are also more common with increasing age, as the cells of the conduction pathway become less efficient. Some are life-threatening medical emergencies that can result in cardiac arrest. In fact, cardiac arrythmias are one of the most common causes of death when travelling to a hospital.
Others cause symptoms such as an abnormal awareness of heart beat (palpitations), and may be merely uncomfortable. These palpitations have also been known to be caused by atrial/ventricular fibrillation, wire faults, and other technical or mechanical issues in cardiac pacemakers/defibrillators. Still others may not be associated with any symptoms at all, but may predispose the patient to a potentially life-threatening stroke or embolism.
The heart valves may also become thickened by fibrosis , leading to heart murmurs and less efficient pumping. In the elderly, ventricular diastolic stiffness can lead to pulmonary circulatory congestion. Aortic stenosis and aortic insufficiency, elevate left ventricular preload to the point where it becomes stiff and noncompliant, and is common in people 75 years of age or older. These elevated pressures are transmitted to the pulmonary vasculature and lead to pulmonary edema.
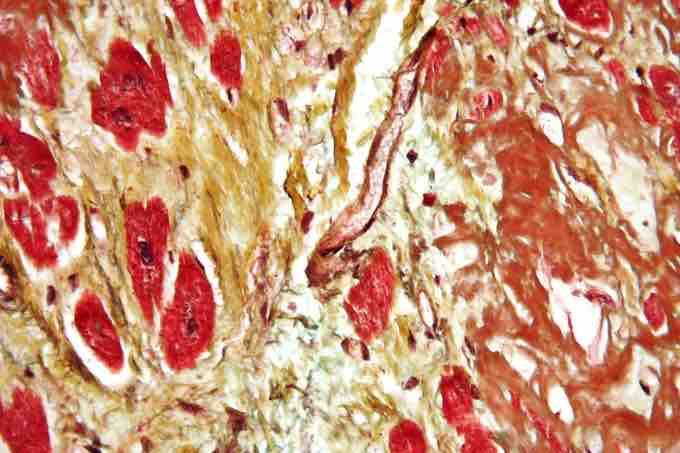
Reticular Fibers
High magnification micrograph of senile cardiac amyloidosis (brown) and fibrosis (yellow). Movat stain (black = nuclei, elastic fibers; yellow = collagen, reticular fibers; blue = ground substance, mucin; bright red = fibrin; red = muscle). Autopsy specimen.