Genital warts (or Condylomata acuminata, venereal warts, anal warts and anogenital warts) is a highly contagious sexually transmitted disease caused by some sub-types of human papillomavirus (HPV ). It is spread through direct skin-to-skin contact during oral, genital, or anal sex with an infected partner. Throat, mouth, and eye genital warts can also be transmitted through oral, genital, or anal sex. Warts are the most easily recognized symptom of genital HPV infection, where types 6 and 11 are responsible for 90% of genital warts cases.
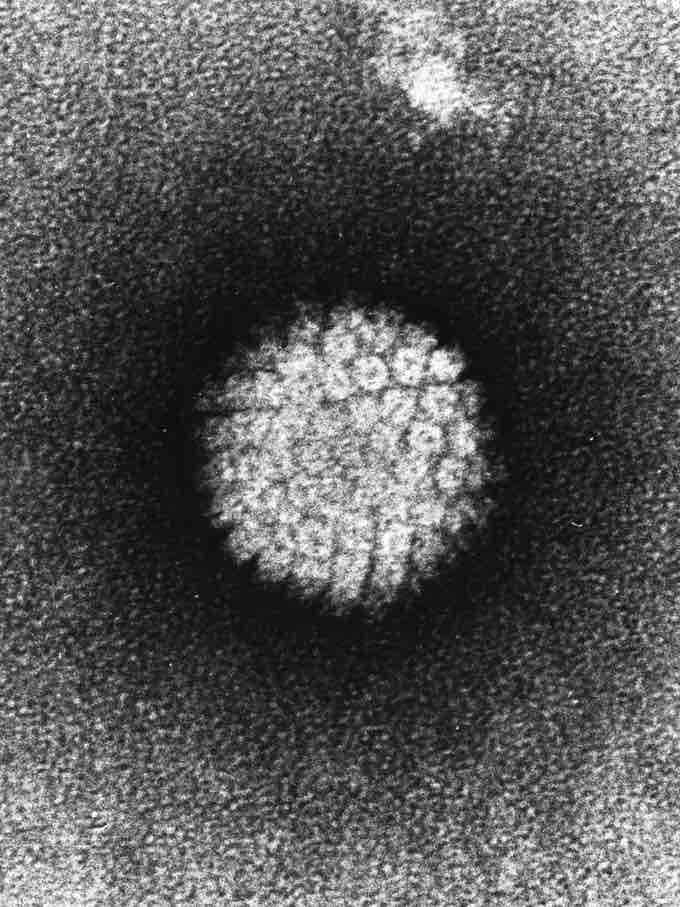
EM of HPV
TEM of papillomavirus.
Although it is estimated that only a "small percentage" (between 1% and 5%) of those infected with genital HPV develop genital warts, those infected can still transmit the virus. Other types of HPV also cause cervical cancer and probably most anal cancers, however it is important to underline that the types of HPV that cause the overwhelming majority of genital warts are not the same as those that can potentially increase the risk of genital or anal cancer. HPV prevalence at any one time has been observed in some studies at 27% over all sexually active people, rising to 45% between the ages of 14 and 19.
Diagnosis
Genital warts, histopathologically, characteristically rise above the skin surface due to enlargement of the dermal papillae, have parakeratosis and the characteristic nuclear changes typical of HPV infections (nuclear enlargement with perinuclear clearing).
Prevention
Gardasil (sold by Merck & Co.) is a vaccine that protects against human papillomavirus types 16, 18, 6, and 11. Types 6 and 11 cause genital warts, while 16 and 18 cause cervical cancer. The vaccine is preventive, not therapeutic, and must be given before exposure to the virus type to be effective, ideally before the beginning of sexual activity. The vaccine is widely approved for use by young women, it is being tested for young men, and has been approved for males in some areas, such as the UK, the US and Canada.
Management
There is no cure for HPV, but there are methods to treat visible warts, which could reduce infectivity, although there are no trials studying the effectiveness of removing visible warts in reducing transmission. Every year, Americans spend $200 million on the treatment of genital warts. Genital warts may disappear without treatment, but sometimes eventually develop a fleshy, small raised growth. There is no way to predict whether they will grow or disappear.
Warts can sometimes be identified because they show up as white when acetic acid is applied, but this method is not recommended on the vulva because microtrauma and inflammation can also show up as acetowhite. Magnifying glasses or colposcope may also be used to aid in identifying small warts. Depending on the sizes and locations of warts (as well as other factors), a doctor will offer one of several ways to treat them. Podofilox is the first-line treatment due to its low cost.Almost all treatments can potentially cause depigmentation or scarring. A 0.15% – 0.5% podophyllotoxin (also called podofilox) solution in a gel or cream. Marketed as Condylox (0.5%), Wartec (0.15%) and Warticon (0.15%), it can be applied by the patient to the affected area and is not washed off. It is the purified and standardized active ingredient of the podophyllin (see below). Podofilox is safer and more effective than podophyllin. Skin erosion and pain are more commonly reported than with imiquimod and sinecatechins. Its use is cycled (2 times per day for 3 days then 4–7 days off); one review states that it should only be used for four cycles.
Imiquimod (Aldara) is a topical immune response cream, applied to the affected area. It causes less local irritation than podofilox but may cause fungal infections (11% in package insert) and flu-like symptoms (less than 5% disclosed in package insert). Sinecatechins (marketed as Veregen and Polyphenon E) is an ointment of catechins (55% epigallocatechin gallate) extracted from green tea and other components. Mode of action is undetermined. It appears to have higher clearance rates than podophyllotoxin and imiquimod and causes less local irritation, but clearance takes longer than with imiquimod. Liquid nitrogen cryosurgery is safe for pregnancy. It kills warts 71–79% of the time, but recurrence is 38% to 73% 6 months after treatment. Local infections have been reported. Trichloroacetic acid (TCA) is less effective than cryosurgery, and is not recommended for use in the vagina, cervix, or urinary meatus. Surgical excision is best for large warts, and has a greater risk of scarring. Laser ablation does not seem to be any more effective than other physician-applied methods, but is often used as a last resort and is extremely expensive. A 20% podophyllin anti-mitotic solution, applied to the affected area and later washed off. However, this crude herbal extract is not recommended for use on vagina, urethra, perianal area, or cervix, and must be applied by a physician.
Reported reactions include nausea, vomiting, fever, confusion, coma, renal failure, ileus, and leukopenia; death has been reported with extensive topical application, or application on mucous membranes. Interferon can be used; it is effective, but it is also expensive and its effect is inconsistent. Electrocauterization can be used; it is an older procedure but recovery time is generally longer. In severe cases of genital warts, treatment may require general or spinal anesthesia. This is a surgical procedure. More effective than cryosurgery and recurrence is at a much lower rate. Oral Isotretinoin is a therapy that has proven effective in experimental use, but is rarely used due to potentially severe side effects. In a small-scale study, low dose oral isotretinoin showed considerable efficacy and may represent an alternative systemic form of therapy for Genital Warts. Yet, albeit this indicative evidence not many studies have been conducted to further confirm the findings. In most countries this therapy is currently unapproved and only used as an alternative therapy if other therapies failed.