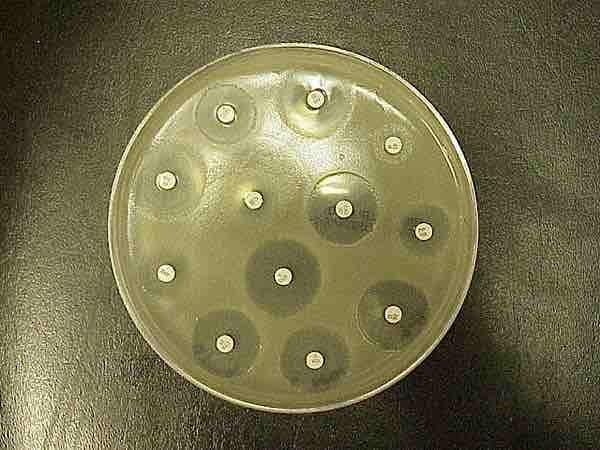
Kirby-Bauer antibiotic testing (also called KB testing or disk diffusion antibiotic sensitivity testing) uses antibiotic-containing wafers or disks to test whether particular bacteria are susceptible to specific antibiotics. First, a pure culture of bacteria is isolated from the patient. Then, a known quantity of bacteria are grown overnight on agar (solid growth media) plates in the presence of a thin wafer that contains a known amount of a relevant antibiotic. If the bacteria are susceptible to the particular antibiotic from a wafer, an area of clear media where bacteria are not able to grow surrounds the wafer, which is known as the zone of inhibition. A larger zone of inhibition around an antibiotic-containing disk indicates that the bacteria are more sensitive to the antibiotic in the disk.
Kirby-Bauer test
In Kirby–Bauer testing, discs containing antibiotics are placed on agar where bacteria are growing, and the antibiotics diffuse out into the agar. If an antibiotic stops the bacteria from growing, one can see circular areas around the wafers where bacteria have not grown.
KB tests are performed under standardized conditions and standard-sized zones of inhibition have been established for each antibiotic. KB test results are usually reported as sensitive, intermediate, or resistant, based on the size of the zone of inhibition. If the observed zone of inhibition is greater than or equal to the size of the standard zone, the microorganism is considered to be sensitive to the antibiotic. Conversely, if the observed zone of inhibition is smaller than the standard size, the microorganism is considered to be resistant. The size of a zone of inhibition in a KB test is inversely related to the minimum inhibitory concentration (MIC), which is the amount of antibiotic required to prevent bacterial growth in an overnight culture. The MIC (in µg/ml) can be calculated from known standard-curve (linear regression) graphs based on the diameter of the observed inhibition zone diameter (in millimeters).
Clinicians can use KB test results to choose appropriate antibiotics to combat a particular infection in a patient. Administering antibiotics that specifically target the particular bacteria that are causing the infection can avoid using broad-spectrum antibiotics, which target many types of bacteria. Thus, clinical application of KB testing results can decrease the frequency with which antibiotic-resistant bacteria evolve.