Dead Space: V/Q Mismatch
The pulmonary circulation pressure is very low compared to that of the systemic circulation; it is also independent of cardiac output. Recruitment is the process of opening airways that normally remain closed when cardiac output increases. As cardiac output increases, the number of capillaries and arteries that are perfused (filled with blood) increases. These capillaries and arteries are not always in use, but are ready if needed. However, at times, there is a mismatch between the amount of air (ventilation, V) and the amount of blood (perfusion, Q) in the lungs. This is referred to as ventilation/perfusion (V/Q) mismatch.
There are two types of V/Q mismatch that produce dead space. Dead space is characterized by regions of broken down or blocked lung tissue. Dead spaces can severely impact breathing due to the reduction in surface area available for gas diffusion. As a result, the amount of oxygen in the blood decreases, whereas the carbon dioxide level increases. Dead space is created when no ventilation and/or perfusion takes place. Anatomical dead space, or anatomical shunt, arises from an anatomical failure, while physiological dead space, or physiological shunt, arises from a functional impairment of the lung or arteries.
An example of an anatomical shunt is the effect of gravity on the lungs. The lung is particularly susceptible to changes in the magnitude and direction of gravitational forces. When someone is standing or sitting upright, the pleural pressure gradient leads to increased ventilation further down in the lung. As a result, the intrapleural pressure is more negative at the base of the lung than at the top; more air fills the bottom of the lung than the top. Likewise, it takes less energy to pump blood to the bottom of the lung than to the top when in a prone position (lying down). Perfusion of the lung is not uniform while standing or sitting. This is a result of hydrostatic forces combined with the effect of airway pressure. An anatomical shunt develops because the ventilation of the airways does not match the perfusion of the arteries surrounding those airways. As a result, the rate of gas exchange is reduced. Note that this does not occur when lying down because in this position, gravity does not preferentially pull the bottom of the lung down. When a healthy individual stands up quickly after lying down for a while, both ventilation and perfusion increase.
A physiological shunt can develop if there is infection or edema in the lung that obstructs an area. This will decrease ventilation but not affect perfusion; therefore, the V/Q ratio changes and gas exchange is affected .
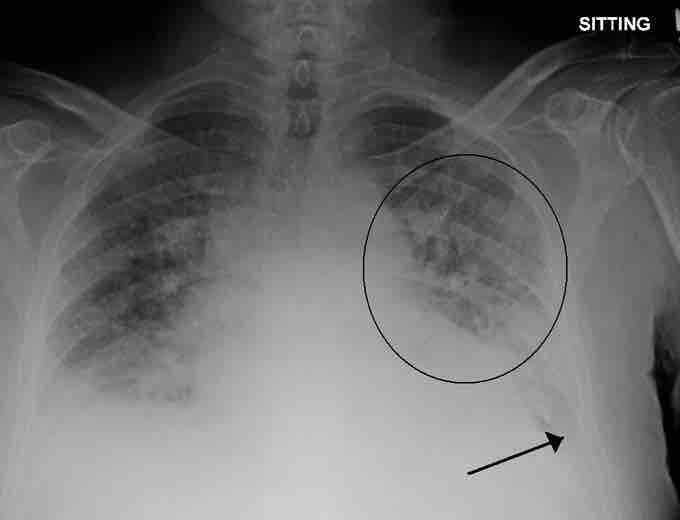
Pulmonary edema
A physiological shunt can develop if there is infection or edema in the lung which decreases ventilation, but does not affect perfusion; thus, the ventilation/perfusion ratio is affected. Pulmonary edema with small pleural effusions on both sides (as shown) can cause changes in the V/Q ratio.
The lung has the capability to compensate for mismatches in ventilation and perfusion. If ventilation is greater than perfusion, the arterioles dilate and the bronchioles constrict, increasing perfusion while reducing ventilation. Likewise, if ventilation is less than perfusion, the arterioles constrict while the bronchioles dilate to correct the imbalance.