Meningitis
Background Information
SOS Children produced this website for schools as well as this video website about Africa. Before you decide about sponsoring a child, why not learn about different sponsorship charities first?
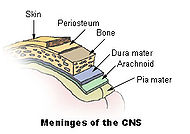
Meningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Meningitis may develop in response to a number of causes, usually bacteria, viruses and other pathogens, but also physical injury, cancer or certain drugs. While some forms of meningitis are mild and resolve on their own, meningitis is a potentially life-threatening condition due to the proximity of the inflammation to the brain and spinal cord. The potential for serious neurological damage or even death necessitates prompt medical attention and evaluation. Infectious meningitis, the most common form, is typically treated with antibiotics and requires close observation. Some forms of meningitis (such as those associated with meningococcus, mumps virus or pneumococcus infections) may be prevented with immunization.
Signs and symptoms
Severe headache is the most common symptom of meningitis (87 percent) followed by nuchal rigidity ("neck stiffness", found in 83%). The classic triad of diagnostic signs consists of nuchal rigidity (being unable to flex the neck forward), sudden high fever and altered mental status. All three features are present in only 44% of all cases of infectious meningitis. Other signs commonly associated with meningitis are photophobia (inability to tolerate bright light), phonophobia (inability to tolerate loud noises), irritability and delirium (in small children) and seizures (in 20-40% of cases). In infants (0-6 months), swelling of the fontanelle (soft spot) may be present.
Nuchal rigidity is the inability to flex the neck forward passively due to increased tone in the neck muscles. Other signs of meningism include Kernig's sign and Brudzinksy's sign. Kernig's sign is typically assessed with the patient lying supine, with one hip flexed to 90 degrees and the knee flexed to 90 degrees. If pain is elicited when the knee is passively extended, and it is not able to reach full extension, this indicates meningism. Brudzinski's sign is used in infants, where forward flexion of the neck may cause involuntary knee and hip flexion. Although commonly tested, the sensitivity and specificity of Kernig's and Brudzinski's tests are limited.
In "meningococcal" meningitis (i.e. meningitis caused by the bacteria Neisseria meningitidis), a rapidly-spreading petechial rash is typical, and may precede other symptoms. The rash consists of numerous small, irregular purple or red spots on the trunk, lower extremities, mucous membranes, conjunctiva, and occasionally on the palms of hands and soles of feet. Other clues to the nature of the cause may be the skin signs of hand, foot and mouth disease and genital herpes, both of which may be associated with viral meningitis.
Meninigitis can be diagnosed after death has occurred. The findings from a post mortum are usually a diffuse (widespread) inflammation of the pia-arachnoid area. Neutrophil leucocytes tend to have migrated to the cerebrospinal fluid and the base of the brain, along with cranial nerves and the spinal cord, may be surrounded with pus—as may the meningeal vessels.
Diagnosis
Investigations
Investigations include blood tests (electrolytes, liver and kidney function, inflammatory markers and a complete blood count) and usually X-ray examination of the chest. The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid (fluid that envelops the brain and the spinal cord) through lumbar puncture (LP). However, if the patient is at risk for a cerebral mass lesion or elevated intracranial pressure (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a lumbar puncture may be contraindicated because of the possibility of fatal brain herniation. In such cases a CT or MRI scan is generally performed prior to the lumbar puncture to exclude this possibility. Otherwise, the CT or MRI should be performed after the LP, with MRI preferred over CT due to its superiority in demonstrating areas of cerebral edema, ischemia, and meningeal inflammation.
During the lumbar puncture procedure, the opening pressure is measured. A pressure of over 180 mm H2O is indicative of bacterial meningitis.
The cerebrospinal fluid (CSF) sample is examined for white blood cells (and which subtypes), red blood cells, protein content and glucose level. Gram staining of the sample may demonstrate bacteria in bacterial meningitis, but absence of bacteria does not exclude bacterial meningitis; microbiological culture of the sample may still yield a causative organism. The type of white blood cell predominantly present predicts whether meningitis is due to bacterial or viral infection. Other tests performed on the CSF sample include latex agglutination test, limulus lysates, or polymerase chain reaction (PCR) for bacterial or viral DNA. If the patient is immunocompromised, testing the CSF for toxoplasmosis, Epstein-Barr virus, cytomegalovirus, JC virus and fungal infection may be performed.
| Condition | Glucose | Protein | Cells |
|---|---|---|---|
| Acute bacterial meningitis | Low | high | high, often > 300/mm³ |
| Acute viral meningitis | Normal | normal or high | mononuclear, < 300/mm³ |
| Tuberculous meningitis | Low | high | pleocytosis, mixed < 300/mm³ |
| Fungal meningitis | Low | high | < 300/mm³ |
| Malignant meningitis | Low | high | usually mononuclear |
| Subarachnoid hemorrhage | Normal | normal, or high | Erythrocytes |

In bacterial meningitis, the CSF glucose to serum glucose ratio is < 0.4. The Gram stain is positive in >60% of cases, and culture in >80%. Latex agglutination may be positive in meningitis due to Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Escherichia coli, Group B Streptococci. Limulus lysates may be positive in Gram-negative meningitis.
Cultures are often negative if CSF is taken after the administration of antibiotics. In these patients, PCR can be helpful in arriving at a diagnosis. It has been suggested that CSF cortisol measurement may be helpful.
Aseptic meningitis refers to non-bacterial causes of meningitis and includes infective etiologies such as viruses and fungi, neoplastic etiologies such as carcinomatous and lymphomatous meningitis, inflammatory causes such as sarcoidosis ( neurosarcoidosis)) and chemical causes such as meningitis secondary to the intrathecal introduction of contrast media.
Although the term "viral meningitis" is often used in any patient with a mild meningeal illness with appropriate CSF findings, certain patients will present with clinical and CSF features of viral meningitis, yet ultimately be diagnosed with one of the other conditions categorized as "aseptic meningitis". This may be prevented by performing PCR or serology on CSF or blood for common viral causes of meningitis ( enterovirus, herpes simplex virus 2 and mumps in those not vaccinated for this).
A related diagnostic and therapeutic conundrum is the "partially treated meningitis", i.e. meningitis symptoms in patients who have already been receiving antibiotics (such as for presumptive sinusitis). In these patients, CSF findings may resemble those of viral meningitis, but antibiotic treatment may need to be continued until there is definitive positive evidence of a viral cause (e.g. a positive enterovirus PCR).
Prediction rules
The Bacterial Meningitis Score predicts reliably whether a child (older than two months) may have infectious meningitis. In children with at least 1 risk factor (positive CSF Gram stain, CSF absolute neutrophil count ≥ 1000 cell/µL, CSF protein ≥ 80 mg/dL, peripheral blood absolute neutrophil count ≥ 10,000 cell/µL, history of seizure before or at presentation time) it had a sensitivity of 100%, specificity of 63.5%, and negative predictive value of 100%.
Causes
Most cases of meningitis are caused by microorganisms, such as viruses, bacteria, fungi, or parasites, that spread into the blood and into the cerebrospinal fluid (CSF). Non-infectious causes include cancers, systemic lupus erythematosus and certain drugs. The most common cause of meningitis is viral, and often runs its course within a few days. Bacterial meningitis is the second most frequent type and can be serious and life-threatening. Numerous microorganisms may cause bacterial meningitis, but Neisseria meningitidis ("meningococcus") and Streptococcus pneumoniae ("pneumococcus") are the most common pathogens in patients without immune deficiency, with meningococcal disease being more common in children. Staphylococcus aureus may complicate neurosurgical operations, and Listeria monocytogenes is associated with poor nutritional state and alcoholism. Haemophilus influenzae (type B) incidence has been much reduced by immunization in many countries. Mycobacterium tuberculosis (the causative agent of tuberculosis) rarely causes meningitis in Western countries but is common and feared in countries where tuberculosis is endemic.
Treatment
Initial treatment
Meningitis is a life-threatening condition and treatment should not be delayed for confirmation if suspected. If a physician is present on scene then treatment should begin immediately with benzylpenicillin. High-flow oxygen should be administered as soon as possible, along with an intravenous fluids if hypotensive or in shock.
Bacterial meningitis
Bacterial meningitis is a medical emergency and has a high mortality rate if untreated. All suspected cases, however mild, need emergency medical attention. Empiric antibiotics must be started immediately, even before the results of the lumbar puncture and CSF analysis are known. Antibiotics started within 4 hours of lumbar puncture will not significantly affect lab results. Adjuvant treatment with corticosteroids reduces rates of mortality, severe hearing loss and neurological sequelae in adults, specifically when the causative agent is Pneumococcus.
| Age group | Causes |
|---|---|
| Neonates | Group B Streptococci, Escherichia coli, Listeria monocytogenes |
| Infants | Neisseria meningitidis, Haemophilus influenzae, Streptococcus pneumoniae |
| Children | N. meningitidis, S. pneumoniae |
| Adults | S. pneumoniae, N. meningitidis, Mycobacteria, Cryptococci |
The choice of antibiotic depends on local advice. In most of the developed world, the most common organisms involved are Streptococcus pneumoniae and Neisseria meningitidis: first line treatment in the UK is a third-generation cephalosporin (such as ceftriaxone or cefotaxime). In those under 3 years of age, over 50 years of age, or immunocompromised, ampicillin should be added to cover Listeria monocytogenes. In the U.S. and other countries with high levels of penicillin resistance, the first line choice of antibiotics is vancomycin and a carbapenem (such as meropenem). In sub-Saharan Africa, oily chloramphenicol or ceftriaxone are often used because only a single dose is needed in most cases.
Staphylococci and gram-negative bacilli are common infective agents in patients who have just had a neurosurgical procedure. Again, the choice of antibiotic depends on local patterns of infection: cefotaxime and ceftriaxone remain good choices in many situations, but ceftazidime is used when Pseudomonas aeruginosa is a problem, and intraventricular vancomycin is used for those patients with intraventricular shunts because of high rates of staphylococcal infection. In patients with intracerebral prosthetic material (metal plates, electrodes or implants, etc.) then sometimes chloramphenicol is the only antibiotic that will adequately cover infection by Staphylococcus aureus (cephalosporins and carbapenems are inadequate under these circumstances).
Once the results of the CSF analysis are known along with the Gram-stain and culture, empiric therapy may be switched to therapy targeted to the specific causative organism and its sensitivities.
- Neisseria meningitidis (Meningococcus) can usually be treated with a 7-day course of IV antibiotics:
- Penicillin-sensitive -- penicillin G or ampicillin
- Penicillin-resistant -- ceftriaxone or cefotaxime
- Prophylaxis for close contacts (contact with oral secretions) -- rifampin 600 mg bid for 2 days (adults) or 10 mg/kg bid (children). Rifampin is not recommended in pregnancy and as such, these patients should be treated with single doses of ciprofloxacin, azithromycin, or ceftriaxone
- Streptococcus pneumoniae (Pneumococcus) can usually be treated with a 2-week course of IV antibiotics:
- Penicillin-sensitive -- penicillin G
- Penicillin-intermediate -- ceftriaxone or cefotaxime
- Penicillin-resistant -- ceftriaxone or cefotaxime + vancomycin
- Listeria monocytogenes is treated with a 3-week course of IV ampicillin + gentamicin.
- Gram negative bacilli -- ceftriaxone or cefotaxime
- Pseudomonas aeruginosa -- ceftazidime
- Staphylococcus aureus
- Methicillin-sensitive -- nafcillin
- Methicillin-resistant -- vancomycin
- Streptococcus agalactiae -- penicillin G or ampicillin
- Haemophilus influenzae -- ceftriaxone or cefotaxime
Viral meningitis
Patients diagnosed with mild viral meningitis may improve quickly enough to not require admission to a hospital, while others may be hospitalized for many more days for observation and supportive care. Overall, the illness is usually much less severe than bacterial meningitis.
Unlike bacteria, viruses cannot be killed by antibiotics. Drugs such as acyclovir may be employed if herpes virus infection is either suspected or demonstrated.
Fungal meningitis
This form of meningitis is rare in otherwise healthy people but is a higher risk in those who have AIDS, other forms of immunodeficiency (an immune system that does not respond adequately to infections) and immunosuppression (immune system malfunction as a result of medical treatment). In AIDS, Cryptococcus neoformans is the most common cause of fungal meningitis; it requires Indian ink staining of the CSF sample for identification of this capsulated yeast. Fungal meningitis is treated with long courses of highly dosed antifungals.
Complications
In children there are several potential disabilities which result from damage to the nervous system. These include sensorineural hearing loss, epilepsy, diffuse brain swelling, hydrocephalus, cerebral vein thrombosis, intra cerebral bleeding and cerebral palsy. Acute neurological complications may lead to adverse consequences. In childhood acute bacterial meningitis deafness is the most common serious complication. Sensorineural hearing loss often develops during first few days of the illness as a result of inner ear dysfunction, but permanent deafness is rare and can be prevented by prompt treatment of meningitis.
Those that contract the disease during the neonatal period and those infected by S. pneumoniae and gram negative bacilli are at greater risk of developing neurological, auditory, or intellectual impairments or functionally important behaviour or learning disorders which can manifest as poor school performance.
In adults central nervous system complications include brain infarction, brain swelling, hydrocephalus, intracerebral bleeding; systemic complications are dominated by septic shock, adult respiratory distress syndrome and disseminated intravascular coagulation. Those who have underlying predisposing conditions e.g. head injury may develop recurrent meningitis. Case-fatality ratio is highest for gram-negative etiology and lowest for meningitis caused by H. influenzae (also a gram negative bacilli). Fatal outcome in patients over 60 years of age is more likely to be from systemic complications e.g. pneumonia, sepsis, cardio-respiratory failure; however in younger individuals it is usually associated with neurological complications. Age more than 60, low Glasgow coma scale at presentation and seizure within 24 hours increase the risk of death among community acquired meningitis.
Prevention
Immunization
Vaccinations against Haemophilus influenzae ( Hib) have decreased early childhood meningitis significantly.
Vaccines against type A and C Neisseria meningitidis, the kind that causes most disease in preschool children and teenagers in the United States, have also been around for a while. Type A is also prevalent in sub-Sahara Africa and W135 outbreaks have affected those on the Hajj pilgrimage to Mecca. Immunisation with the ACW135Y vaccine against four strains is now a visa requirement for taking part in the Hajj.
Vaccines against type B Neisseria meningitidis are much harder to produce, as its capsule is very weakly immunogenic masking its antigenic proteins. There is also a risk of autoimmune response, and the porA and porB proteins on Type B resemble neuronal molecules. A vaccine called MeNZB for a specific strain of type B Neisseria meningitidis prevalent in New Zealand has completed trials and is being given to many people in the country under the age of 20 free of charge. There is also a vaccine, MenBVac, for the specific strain of type B meningoccocal disease prevalent in Norway, and another specific vaccine for the strain prevalent in Cuba. According to reports released in May 2008, Novartis is in the advanced stages of testing a general meningococcus type B vaccine.
Pneumococcal polysaccharide vaccine against Streptococcus pneumoniae is recommended for all people 65 years of age or older. Pneumococcal conjugate vaccine is recommended for all newborns starting at 6 weeks - 2 months, American Academy of Pediatrics (AAP) recommendations.
Mumps vaccination has led to a sharp decline in mumps virus associated meningitis, which prior to vaccination occurred in 15% of all cases of mumps.
According to reports released in May 2008, Novartis is in the advanced stages of testing a general meningococcus type B vaccine.
Prophylaxis
In cases of meningococcal meningitis, prophylactic treatment of close relatives with antibiotics (e.g. rifampicin, ciprofloxacin or ceftriaxone) may reduce the risk of further cases.
Epidemiology
Meningitis can affect anyone in any age group, from the newborn to the elderly.
The "Meningitis Belt" is an area in sub-Saharan Africa which stretches from Senegal in the west to Ethiopia in the east in which large epidemics of meningococcal meningitis occur (this largely coincides with the Sahel region). It contains an estimated total population of 300 million people. The largest epidemic outbreak was in 1996, when over 250,000 cases occurred and 25,000 people died as a consequence of the disease.
History
Meningitis was first described in the 1020s in Avicenna's The Canon of Medicine, and again more accurately by Avenzoar of al-Andalus in the 12th century. Symptoms of the disease were also noted in 1805 by the Swiss Gabinetto Vieusseux (a scientific-literary association) during an outbreak in Geneva, Switzerland. In 1887, Dr. Anton Weichselbaum (1845-1920) of Vienna became the first to isolate the specific germ, meningococcus.
In the 19th century, meningitis was a scourge of the Japanese imperial family, playing the largest role in the horrendous pre-maturity mortality rate the family endured. In the mid-1800s, only the Emperor Kōmei and two of his siblings reached maturity out of fifteen total children surviving birth. Kōmei's son, the Emperor Meiji, was one of two survivors out of Kōmei's six children, including an elder brother of Meiji who would have taken the throne had he lived to maturity. Five of Meiji's 15 children survived, including only his third son, Emperor Taishō, who was feeble-minded, perhaps as a result of having contracted meningitis himself. By Emperor Hirohito's generation the family was receiving modern medical attention. As the focal point of tradition in Japan, during the Tokugawa Shogunate the family was denied modern "Dutch" medical treatment then in use among the upper caste; despite extensive modernization during the Meiji Restoration the Emperor insisted on traditional medical care for his children.