The Types of Ventilation Rates
In respiratory physiology, the ventilation rate is the rate at which gas enters or leaves the lung. Ventilation is generally expressed as volume of air times a respiratory rate.
The volume of air can refer to tidal volume (the amount inhaled in an average breath) or something more specific, such as the volume of dead space in the airways. The three main types of ventilation rates used in respiratory physiology are:
- Minute ventilation (VE):
The amount of air entering the lungs per minute. It can be defined as
$VE=TidalVolume*BreathsPerMinute$ - Alveolar ventilation (VA):
The amount of gas per unit of time that reaches the alveoli and becomes involved in gas exchange. It is defined
as
$VA=(Tidal Volume-Dead Space Volume)* Respiratory Rate$ - Dead space ventilation (VD):
The amount of air per unit of time that is not involved in gas exchange, such as the air that remains in the conducting zones. It
is defined as
$VD=DeadSpaceVolume*Respiratory Rate$ .
Additionally, minute ventilation can be described as the sum of alveolar and dead space ventilation, provided that the respiratory rate used to derive them is in terms of breaths per minute.
The three types of ventilation are mathematically linked to one another, so changes in one ventilation rate can cause the change of the other. This is most apparent in changes of the dead space volume. Breathing through a snorkeling tube and having a pulmonary embolism both increase the amount of dead space volume (through anatomical versus alveolar dead space respectively), which will reduce alveolar ventilation.
Alveolar ventilation is the most important type of ventilation for measuring how much oxygen actually gets into the body, which can initiate negative feedback mechanisms to try and increase alveolar ventilation despite the increase in dead space. In particular, the body will generally attempt to combat increased dead space by raising the frequency of breaths to try and maintain sufficient levels of alveolar ventilation.
Partial Pressure of Gasses
When gasses dissolve in the bloodstream during ventilation, they are generally described by the partial pressure of the gasses. Partial pressure more specifically refers to the relative concentration of those gasses by the pressure they exert in a dissolved state.
In respiratory physiology, PAO2 and PACO2,refer to the partial pressures of oxygen and carbon dioxide in the alveoli.
PaO2 and PaCO2 refer to the partial pressures of oxygen and carbon dioxide within arterial blood. Differences in partial pressures of gasses between the alveolar air and the blood stream are the reason that gas exchange occurs by passive diffusion.
Under normal conditions, PAO2 is about 100 mmHg, while PaO2 is 80–100 mmHg in systemic arteries, but 40–50 mmHg in the deoxygenated blood of the pulmonary artery going to the lungs.
Recall that gasses travel from areas of high pressure to areas of low pressure, so the greater pressure of oxygen in the alveoli compared to that of the deoxygenated blood explains why oxygen can passively diffuse into the bloodstream during gas exchange.
Conversely, PACO2 is 35 mmHg, while PaCO2 is about 40–45 mmHG in systemic arteries and 50 mmHg in the pulmonary artery. The partial pressure, and thus concentration of carbon dioxide, is greater in the in the capillaries of the alveoli compared to the alveolar air, so carbon dioxide will passively diffuse from the bloodstream into the alveoli during gas exchange.
Additionally, because PaCO2 is an indicator of the concentration of carbon dioxide in arterial blood, it can be used to measure blood pH and identify cases of respiratory acidosis and alkalkosis.
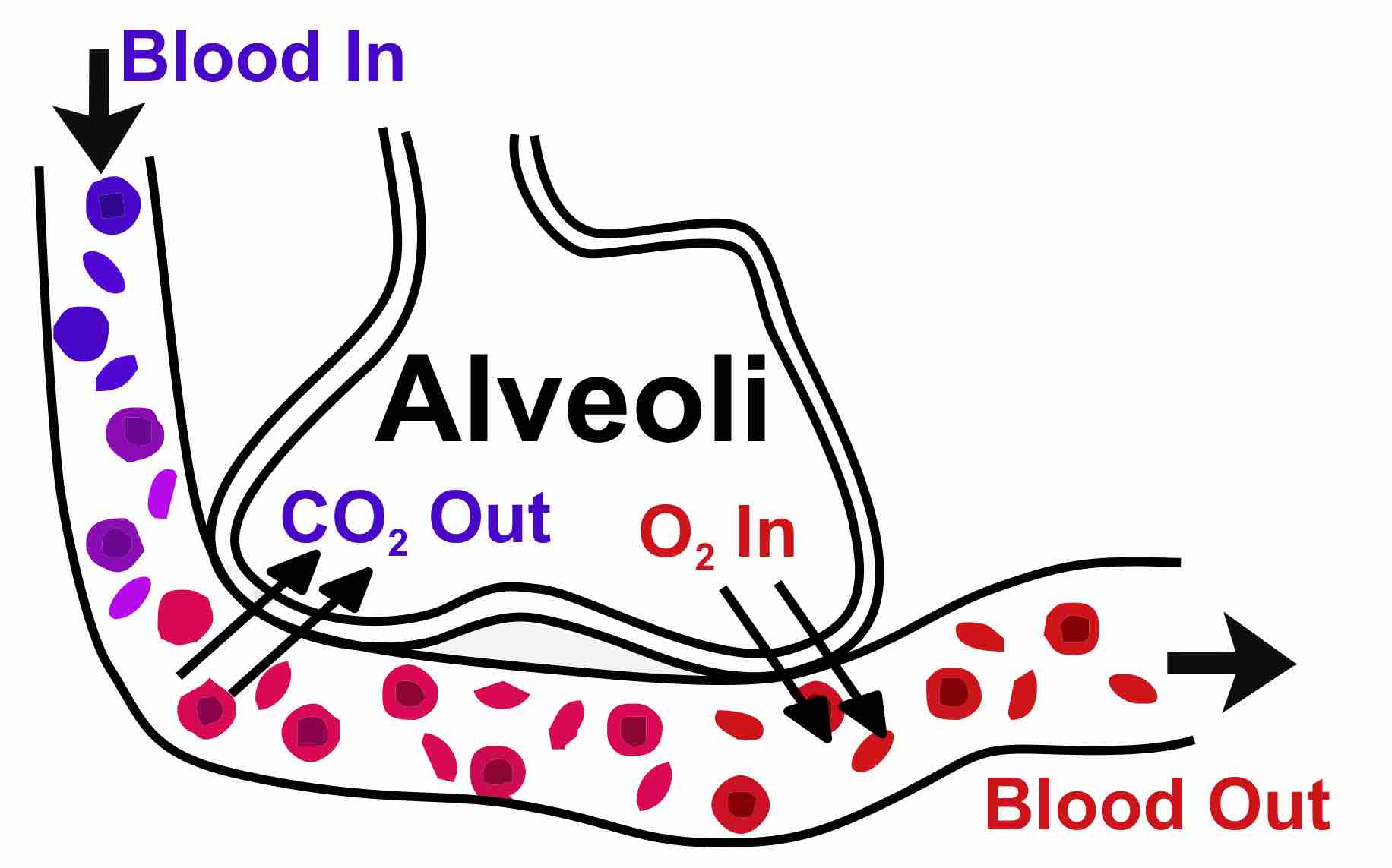
Gaseous Exchange in the Lungs
Diagram of gas exchange in the lungs.