Antigen presentation is a process in the body's immune system by which macrophages, dendritic cells and other cell types capture antigens, then enable their recognition by T-cells. The basis of adaptive immunity lies in the capacity of immune cells to distinguish between the body's own cells and infectious pathogens. The host's cells express "self" antigens that identify them as such. These antigens are different from those in bacteria ("non-self" antigens) or in virally-infected host cells ("missing-self"). The ability of the adaptive immune system to survey for infection requires specialized pathways of enabling recognition of pathogen-derived antigens by T cells.
Activation of T Cells
Unlike B cells, T cells fail to recognize antigens in the absence of antigen presentation, with the important exception of the superantigens. The T cell receptor is restricted to recognizing antigenic peptides only when bound to appropriate molecules of the major histocompatibility complex (MHC), also known in humans as Human leukocyte antigen (HLA). Most cells are capable of presenting antigens and activating the adaptive response. Some cells, however, are specially equipped to acquire and present antigen, and prime naive T cells. Dendritic cells, B cells and macrophages play a major role in the innate response, also acting as professional antigen-presenting cells (APC). These professional APCs are equipped with special immunostimulatory receptors that allow for enhanced activation of T cells.
Several different types of T cell can be activated by professional APCs, and each type of T cell is specially equipped to deal with different pathogens, whether the pathogen is bacterial, viral or a toxin. The type of T cell activated, and therefore the type of response generated, depends in part on the context in which the antigen was first encountered by the APC. Antigen presentation stimulates T cells to become either "cytotoxic" CD8+ cells or "helper" CD4+ cells. Intracellular antigens are produced mainly by viruses replicating within a host cell, though antigens here can also derive from cytoplasmic bacteria or the host cell's own proteins. The host cell digests cytoplasmic proteins by a specialized enzyme complex, the proteasome, into small peptides. A specialized carrier, the Transporter associated with Antigen Processing (TAP) complex moves the peptide into the endoplasmic reticulum, allowing the antigenic peptide to be coupled to an MHC Class I molecule and transported to the cell surface.
MHC Class I molecules present antigen to CD8+ cytotoxic T cells. With the exception of some cell types (such as erythrocytes), Class I MHC is expressed by almost all host cells. Cytotoxic T cells (also known as TC, killer T cell, or cytotoxic T-lymphocyte (CTL)) are a population of T cells that are specialized for inducing the death of other cells. Recognition of antigenic peptides through Class I by CTLs leads to the killing of the target cell, which is infected by virus, intracytoplasmic bacterium, or are otherwise damaged or dysfunctional.
Dentritic Cells (DCs)
Dendritic cells (DCs) phagocytose exogenous pathogens such as bacteria, parasites, and toxins in the tissues and then migrate, via chemotactic signals, to T cell-enriched lymph nodes. During migration, DCs undergo a process of maturation in which they lose phagocytic capacity and develop an increased ability to communicate with T-cells in the lymph nodes. This maturation process is dependent on signaling from other pathogen-associated molecular pattern (PAMP) molecules through pattern recognition receptors, such as the members of the Toll-like receptor family.
The DC uses lysosome-associated enzymes to digest pathogen-associated proteins into smaller peptides. In the lymph node, the DC will display these antigenic peptides on its surface by coupling them to MHC Class II molecules. This MHC:antigen complex is then recognized by T cells passing through the lymph node. Exogenous antigens are usually displayed on MHC Class II molecules, which interact with CD4+ helper T cells. CD4+ lymphocytes, or TH, are immune response mediators, and play an important role in establishing and maximizing the capabilities of the adaptive immune response. Expression of Class II is more restricted than Class I. High levels of Class II are found on dendritic cells, but can also be observed on activated macrophages, B cells, and several other host cell types in inflammatory conditions.
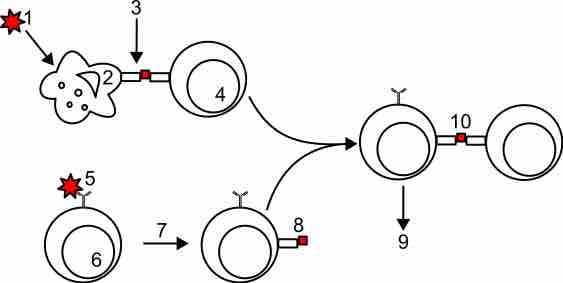
Antigen presentation
In the upper pathway; foreign protein or antigen (1) is taken up by an antigen-presenting cell (2). The antigen is processed and displayed on a MHC II molecule (3), which interacts with a T helper cell (4). In the lower pathway; whole foreign proteins are bound by membrane antibodies (5) and presented to B lymphocytes (6), which process (7) and present antigen on MHC II (8) to a previously activated T helper cell (10), spurring the production of antigen-specific antibodies (9).