Phagocytosis is the process by which a cell takes in particles such as bacteria, parasites, dead host cells, and cellular and foreign debris. It involves a chain of molecular processes. Phagocytosis occurs after the foreign body, a bacterial cell, for example, has bound to molecules called "receptors" that are on the surface of the phagocyte. The phagocyte then stretches itself around the bacterium and engulfs it. Phagocytosis of bacteria by human neutrophils takes on average nine minutes to occur. Once inside the phagocyte, the bacterium is trapped in a compartment called a phagosome. Within one minute the phagosome merges with either a lysosome or a granule, to form a phagolysosome. The bacterium is then subjected to an overwhelming array of killing mechanisms and is dead a few minutes later. Dendritic cells and macrophages, on the other hand, are not so fast, and phagocytosis can take many hours in these cells. Macrophages are slow and untidy eaters; they engulf huge quantities of material and frequently release some undigested material back into the tissues. This debris serves as a signal to recruit more phagocytes from the blood. Phagocytes have voracious appetites; scientists have even fed macrophages with iron filings and then used a small magnet to separate them from other cells.
All phagocytes, and especially macrophages, exist in degrees of readiness. Macrophages are usually relatively dormant in the tissues and proliferate slowly. In this semi-resting state, they clear away dead host cells and other non-infectious debris and rarely take part in antigen presentation. But, during an infection, they receive chemical signals—usually interferon gamma—which increases their production of MHC II molecules and which prepares them for presenting antigens. In this state, macrophages are good antigen presenters and killers. However, if they receive a signal directly from an invader, they become "hyperactivated", stop proliferating, and concentrate on killing. Their size and rate of phagocytosis increases—some become large enough to engulf invading protozoa. In the blood, neutrophils are inactive but are swept along at high speed. When they receive signals from macrophages at the sites of inflammation, they slow down and leave the blood. In the tissues, they are activated by cytokines and arrive at the battle scene ready to kill.
Neutrophils
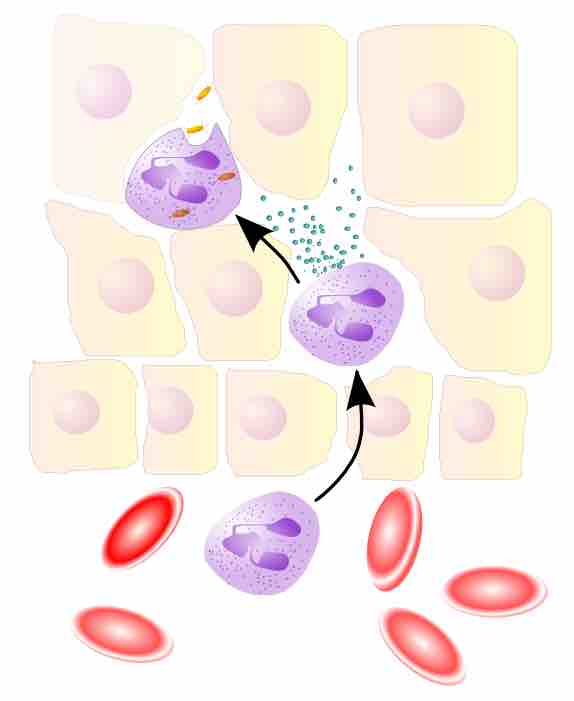
Neutrophils move through the blood to the site of infection.
When an infection occurs, a chemical "SOS" signal is given off to attract phagocytes to the site. These chemical signals may include proteins from invading bacteria, clotting system peptides, complement products, and cytokines that have been given off by macrophages located in the tissue near the infection site. Another group of chemical attractants are cytokines that recruit neutrophils and monocytes from the blood. To reach the site of infection, phagocytes leave the bloodstream and enter the affected tissues. Signals from the infection cause the endothelial cells that line the blood vessels to make a protein called selectin, which neutrophils stick to when they pass by. Other signals called vasodilators loosen the junctions connecting endothelial cells, allowing the phagocytes to pass through the wall. Chemotaxis is the process by which phagocytes follow the cytokine "scent" to the infected spot. Neutrophils travel across epithelial cell-lined organs to sites of infection, and although this is an important component of fighting infection, the migration itself can result in disease-like symptoms. During an infection, millions of neutrophils are recruited from the blood, but they die after a few days.