Periodontal disease is a type of disease that affects one or more of the periodontal tissues, which include:
- the cementum, or the outer layer of the roots of teeth
- the gingiva, or gum tissue
- the alveolar bone, or the bony sockets into which the teeth are anchored
- the periodontal ligament, which are the connective tissue fibers that run between the cementum and the alveolar bone.
While many different diseases affect the tooth-supporting structures, plaque-induced inflammatory lesions make up the vast majority of periodontal diseases and have traditionally been divided into two categories: peridontitis or gingivitis.
Peridontitis
Periodontitis is an inflammatory disease affecting the periodontium, or the tissues that surround and support the teeth. Periodontitis involves progressive loss of the alveolar bone around the teeth, and if left untreated, can lead to the loosening and subsequent loss of teeth . Periodontitis is caused by microorganisms that adhere to and grow on the tooth's surfaces, along with an overly aggressive immune response against these microorganisms.

Periodontal disease
This radiograph shows significant bone loss between the two roots of a tooth (black region). The spongy bone has receded due to infection under the tooth, reducing the bony support for the tooth.
In the early stages, periodontitis has very few symptoms and in many individuals the disease has progressed significantly before they seek treatment. Symptoms may include the following:
- Redness or bleeding of gums while brushing teeth, using dental floss, or biting into hard food
- Gum swelling that recurs
- Spitting out blood after brushing teeth
- Halitosis, or bad breath, and a persistent metallic taste in the mouth
- Gingival recession, resulting in apparent lengthening of teeth
- Deep pockets between the teeth and the gums, that are sites where the attachment has been gradually destroyed by collagen-destroying enzymes, known as collagenases
- Loose teeth, in the later stages
The gingival inflammation and bone destruction of peridontitis are largely painless. Hence, people may wrongly assume that painless bleeding after teeth cleaning is insignificant, although this may be a symptom of progressing periodontitis in that patient.
A diagnosis of periodontitis is established by inspecting the soft gum tissues around the teeth with a probe and by evaluating the patient's x-ray films to determine the amount of bone loss around the teeth.
Gingivitis
Gingivitis, or inflammation of the gums, is a non-destructive peridontal disease . The primary cause of gingivitis is poor oral hygiene which leads to the accumulation of bacterial matrix at the gum line, called dental plaque. Other contributors are poor nutrition and underlying medical issues such as diabetes.

Gingivitis
Severe gingivitis before (top) and after (bottom) treatment.
In some people, gingivitis progresses to periodontitis –- with the destruction of the gingival fibers, the gum tissues separate from the tooth, forming pockets between the tooth and gum. Subgingival microorganism (those that exist under the gum line) colonize the periodontal pockets and cause further inflammation in the gum tissues and progressive bone loss.
If left undisturbed, microbic plaque calcifies to form calculus, which is commonly called tartar. Calculus above and below the gum line must be removed completely by the dental hygienist or dentist to treat gingivitis and periodontitis. Although the primary cause of both gingivitis and periodontitis is the microbic plaque that adheres to the tooth surface, there are many other modifying factors. A very strong risk factor is one's genetic susceptibility. Several conditions and diseases, including Down syndrome, diabetes, and other diseases that affect one's resistance to infection also increase susceptibility to periodontitis.
Prevention
Daily oral hygiene measures to prevent periodontal disease include:
- Brushing teeth properly at least twice daily, with the patient attempting to direct the toothbrush bristles underneath the gum-line, to help disrupt the bacterial-mycotic growth and formation of subgingival plaque.
- Flossing daily and using interdental brushes as well as cleaning behind the last tooth, the third molar, in each quarter.
- Using an antiseptic mouthwash. Chlorhexidine gluconate-based mouthwash in combination with careful oral hygiene may cure gingivitis, although they cannot reverse any attachment loss due to periodontitis.
- Using periodontal trays to maintain dentist-prescribed medications at the source of the disease. The use of trays allows the medication to stay in place long enough to penetrate the biofilms where the microorganism are found.
Regular dental check-ups and professional teeth cleaning as required. Dental check-ups serve to monitor the person's oral hygiene methods and levels of attachment around teeth, identify any early signs of periodontitis, and monitor response to treatment.
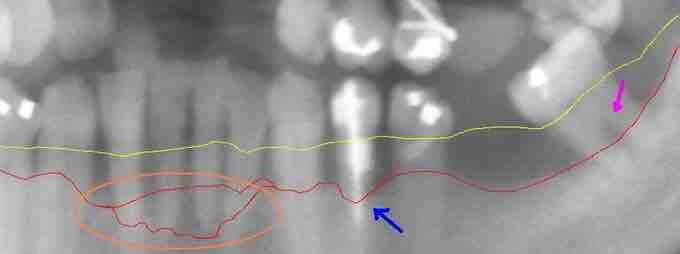
Extensive periodontal disease
This section from a panoramic x-ray film depicts the teeth of the lower left quadrant, exhibiting generalized severe bone loss of 30–80%. The red line depicts the existing bone level, and the yellow line depicts where the gingiva was originally (1–2 mm above the bone), prior to the patient developing periodontal disease. The pink arrow, on the right, points to a furcation involvement, or the loss of enough bone to reveal the location at which the individual roots of a molar begin to branch from the single root trunk; this is a sign of advanced periodontal disease.