The Role of Race in Health
Health disparities refer to gaps in the quality of health and healthcare across racial and ethnic groups. Race and health research, often done in the United States, has found both current and historical racial differences in the frequency, treatments, and availability of treatments for several diseases. This can add up to significant group differences in variables such as life expectancy. Many explanations for such differences have been argued, including socioeconomic factors, lifestyle, social environment, and access to preventive health-care services, among other environmental differences.
In multiracial societies such as the United States, racial groups differ greatly in regard to social and cultural factors such as socioeconomic status, healthcare, diet, and education. There is also the presence of racism which some see as a very important explaining factor. Some argue that for many diseases racial differences would disappear if all environmental factors could be controlled for. Race-based medicine is the term for medicines that are targeted at specific ethnic clusters, which are shown to have a propensity for a certain disorder. Critics are concerned that the trend of research on race specific pharmaceutical treatments will result in inequitable access to pharmaceutical innovation, and smaller minority groups may be ignored.
Health disparities based on race also exist. Similar to the difference in life expectancy found between the rich and the poor, affluent white women live 14 years longer in the U.S. (81.1 years) than poor black men (66.9 years). There is also evidence that blacks receive less aggressive medical care than whites, similar to what happens with women compared to men. Black men describe their visits to doctors as stressful, and report that physicians do not provide them with adequate information to implement the recommendations they are given.
Another contributor to the overall worse health of blacks is the incident of HIV/AIDS; the rate of new AIDS cases is ten times higher among blacks than whites, and blacks are 20 times as likely to have HIV/AIDS as are whites. Health disparities are well documented in minority populations such as African Americans, Native Americans, Asian Americans, and Latinos. When compared to European Americans, these minority groups have higher incidence of chronic diseases, higher mortality, and poorer health outcomes. Minorities also have higher rates of cardiovascular disease, HIV/AIDS, and infant mortality than whites. American ethnic groups can exhibit substantial average differences in disease incidence, disease severity, disease progression, and response to treatment.
Infant mortality is another place where racial disparities are quite evident. In fact, infant mortality rates are 14 of every 1000 births for black, non-Hispanics compared to 6 of every 1000 births for whites. Another disparity is access to health care and insurance. In California, more than half (59 percent) of Hispanics go without health care. Also, almost 25 percent of Latinos do not have health insurance, as opposed to 10 percent of Whites.
There is a controversy regarding race as a method for classifying humans. The continued use of racial categories has been criticized. Apart from the general controversy regarding race, some argue that the continued use of racial categories in health care, and as risk factors, could result in increased stereotyping and discrimination in society and health services. There is general agreement that a goal of health-related genetics should be to move past the weak surrogate relationships of racial health disparity and get to the root causes of health and disease. This includes research which strives to analyze human genetic variation in smaller groups across the world.
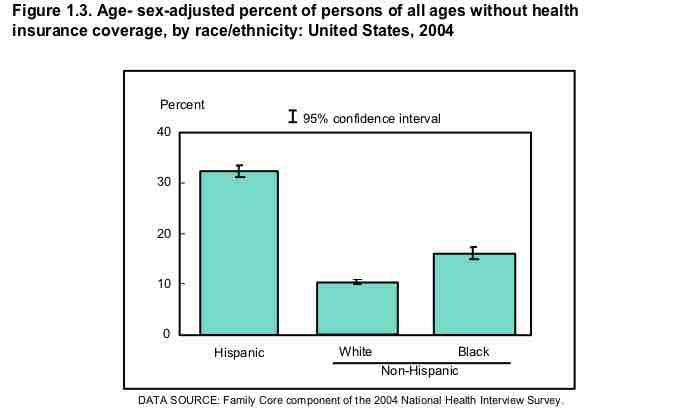
Percentage Without Insurance, Based on Race
Age-sex adjusted percent of persons of all ages without health insurance coverage, by race/ethnicity, United States, 2004