The lungs are a highly elastic organ capable of expanding to a much larger volume during inflation. While the volume of the lungs is proportional to the pressure of the pleural cavity as it expands and contracts during breathing, there is a risk of over-inflation of the lungs if inspiration becomes too deep for too long. Physiological mechanisms exist to prevent over-inflation of the lungs.
The Hering–Bauer Reflex
The Hering–Breuer reflex (also called the inflation reflex) is triggered to prevent over-inflation of the lungs. There are many stretch receptors in the lungs, particularly within the pleura and the smooth muscles of the bronchi and bronchioles, that activate when the lungs have inflated to their ideal maximum point.
These stretch receptors are mechanoreceptors, which are a type of sensory receptor that specifically detects mechanical pressure, distortion, and stretch, and are found in many parts of the human body, especially the lungs, stomach, and skin. They do not detect fine-touch information like most sensory receptors in the human body, but they do create a feeling of tension or fullness when activated, especially in the lungs or stomach.
When the lungs are inflated to their maximum volume during inspiration, the pulmonary stretch receptors send an action potential signal to the medulla and pons in the brain through the vagus nerve.
The pneumotaxic center of the pons sends signals to inhibit the apneustic center of the pons, so it doesn't activate the inspiratory area (the dorsal medulla), and the inspiratory signals that are sent to the diaphragm and accessory muscles stop. This is called the inflation reflex.
As inspiration stops, expiration begins and the lung begins to deflate. As the lungs deflate the stretch receptors are deactivated (and compression receptors called proprioreceptors may be activated) so the inhibitory signals stop and inhalation can begin again—this is called the deflation reflex.
Early physiologists believed this reflex played a major role in establishing the rate and depth of breathing in humans. While this may be true for most animals, it is not the case for most adult humans at rest. However, the reflex may determine the breathing rate and depth in newborns and in adult humans when tidal volume is more than 1 L, such as when exercising.
Additionally, people with emphysema have an impaired Hering–Bauer reflex due to a loss of pulmonary stretch receptors from the destruction of lung tissue, so their lungs can over-inflate as well as collapse, which contributes to shortness of breath.
Sinus Arrhythmia
As the Hering–Bauer reflex uses the vagus nerve as its neural pathway, it also has a few cardiovascular system effects because the vagus nerve also innervates the heart.
During stretch receptor activation, the inhibitory signal that travels through the vagus nerve is also sent to the sinus-atrial node of the heart. Its stimulation causes a short-term increase in resting heart rate, which is called tachycardia.
The heart rate returns to normal during expiration when the stretch receptors are deactivated. When this process is cyclical it is called a sinus arrhythmia, which is a generally normal physiological phenomenon in which there is short-term tachycardia during inspiration.
Sinus arryhthmias do not occur in everyone, and are more common in youth. The sensitivity of the sinus-atrial node to the inflation reflex is lost over time, so sinus arryhthmias are less common in older people.
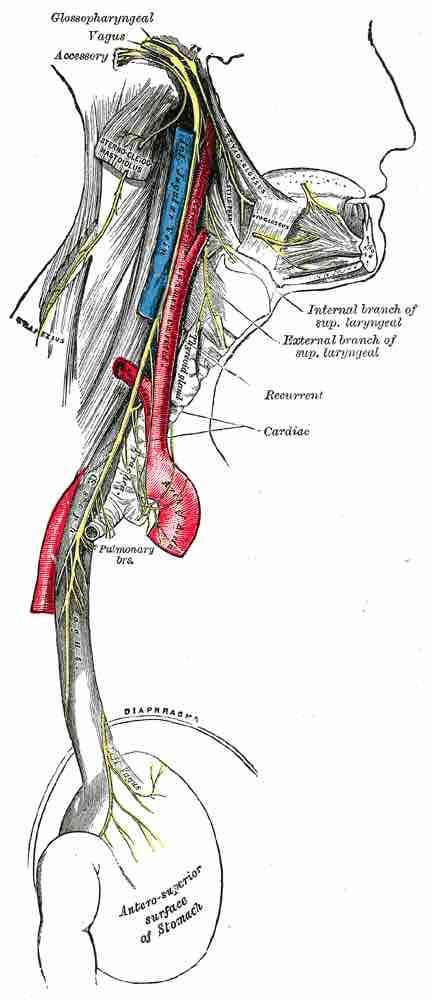
Cardiac and respiratory branches of the vagus nerve
The vagus nerve is the neural pathway for stretch receptor regulation of breathing.