Gas Exchange across the Alveoli
In the human body, oxygen is used by cells of the body's tissues to produce ATP, while carbon dioxide is produced as a waste product. The ratio of carbon dioxide production to oxygen consumption is referred to as the respiratory quotient (RQ), which typically varies between 0.7 and 1.0. If glucose alone were used to fuel the body, the RQ would equal one, as one mole of carbon dioxide would be produced for every mole of oxygen consumed. Glucose, however, is not the only fuel for the body; both proteins and fats are used as well. Since glucose, proteins, and fats are used as fuel sources, less carbon dioxide is produced than oxygen is consumed; the RQ is, on average, about 0.7 for fat and about 0.8 for protein.
The RQ is a key factor because it is used to calculate the partial pressure of oxygen in the alveolar spaces within the lung: the alveolar PO2 (PALVO2). The lungs never fully deflate with an exhalation; therefore, the inspired air mixes with this residual air, lowering the partial pressure of oxygen within the alveoli. This results in a lower concentration of oxygen in the lungs than is found in the air outside the body. When the RQ is known, the partial pressure of oxygen in the alveoli can be calculated: alveolar PO2 = inspired PO2−((alveolar PO2)/RQ)
In the lungs, oxygen diffuses out of the alveoli and into the capillaries surrounding the alveoli. Oxygen (about 98 percent) binds reversibly to the respiratory pigment hemoglobin found in red blood cells. These red blood cells carry oxygen to the tissues where oxygen dissociates from the hemoglobin, diffusing into the cells of the tissues. More specifically, alveolar PO2 is higher in the alveoli (PALVO2=100mmHg) than blood PO2 in the capillaries (40mmHg). Since this pressure gradient exists, oxygen can diffuse down its pressure gradient, moving out of the alveoli and entering the blood of the capillaries where O2 binds to hemoglobin. At the same time, alveolar PCO2 is lower (PALV CO2=40mmHg) than blood PCO2 (45mmHg). Due to this gradient, CO2 diffuses down its pressure gradient, moving out of the capillaries and entering the alveoli.
Oxygen and carbon dioxide move independently of each other; they diffuse down their own pressure gradients. As blood leaves the lungs through the pulmonary veins, the venous PO2=100mmHg, whereas the venous PCO2=40mmHg. As blood enters the systemic capillaries, the blood will lose oxygen and gain carbon dioxide because of the pressure difference between the tissues and blood. In systemic capillaries, PO2=100mmHg, but in the tissue cells, PO2=40mmHg. This pressure gradient drives the diffusion of oxygen out of the capillaries and into the tissue cells. At the same time, blood PCO2=40mmHg and systemic tissue PCO2=45mmHg. The pressure gradient drives CO2 out of tissue cells and into the capillaries. The blood returning to the lungs through the pulmonary arteries has a venous PO2=40mmHg and a PCO2=45mmHg. The blood enters the lung capillaries where the process of exchanging gases between the capillaries and alveoli begins again .
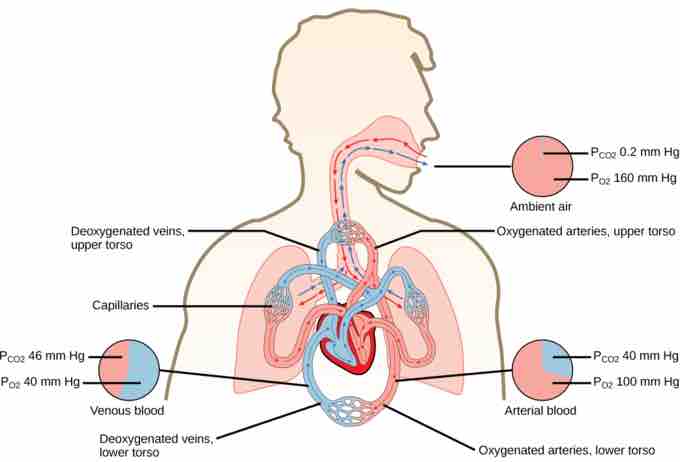
Partial pressures
The partial pressures of oxygen and carbon dioxide change as blood moves through the body.
In short, the change in partial pressure from the alveoli to the capillaries drives the oxygen into the tissues and the carbon dioxide into the blood from the tissues. The blood is then transported to the lungs where differences in pressure in the alveoli result in the movement of carbon dioxide out of the blood into the lungs and oxygen into the blood.